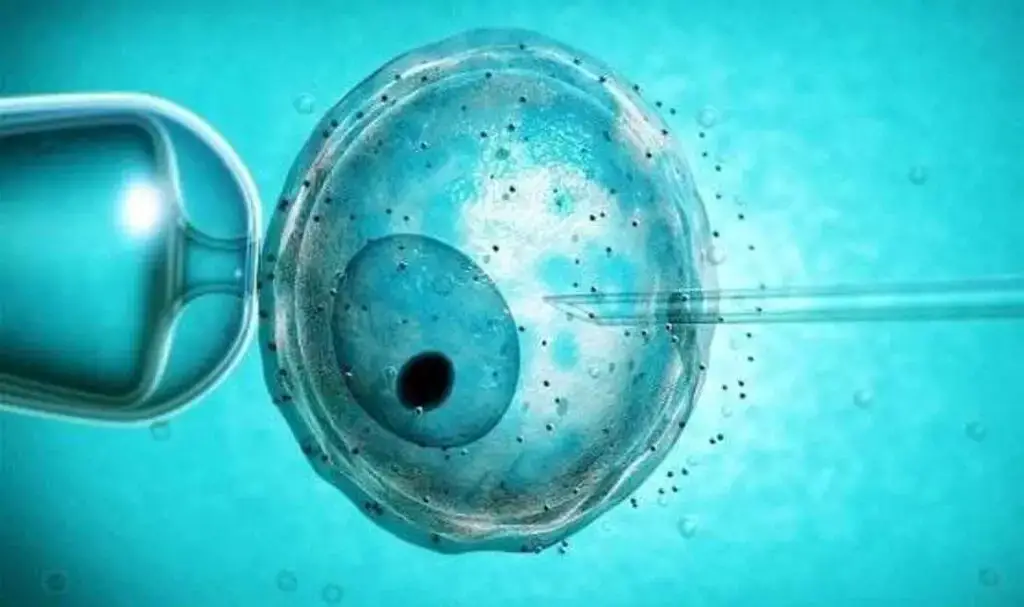
Embarking on the journey of assisted reproductive technology (ART) to achieve pregnancy often involves navigating the choices between fresh embryo transfer (ET) and frozen embryo transfer (FET). Each approach has its unique set of considerations, advantages, and potential outcomes. Understanding the differences between fresh and frozen embryo transfer is crucial for individuals and couples undergoing fertility treatments.
Fresh Embryo Transfer:
In a traditional in vitro fertilization (IVF) cycle, fresh embryo transfer involves the immediate transfer of embryos into the uterus shortly after fertilization. Here’s an exploration of the key aspects of fresh embryo transfer: In a fresh IVF cycle, the timing of embryo transfer is synchronized with the recipient’s natural or artificially induced menstrual cycle. This means that the transfer occurs shortly after the eggs are retrieved and fertilized in the laboratory.
Fresh IVF cycles typically involve ovarian stimulation, where medications are administered to stimulate the ovaries to produce multiple eggs. These eggs are then retrieved for fertilization. The goal is to maximize the number of viable embryos for transfer and potential implantation. The embryos selected for transfer are introduced into the uterus soon after fertilization. This rapid transfer aligns with the natural timeline of embryo development and implantation.
Risk of Ovarian Hyperstimulation Syndrome (OHSS):
Ovarian hyperstimulation syndrome is a potential risk associated with fresh IVF cycles, particularly when a high number of eggs are stimulated and retrieved. OHSS can lead to abdominal discomfort, bloating, and in severe cases, fluid accumulation in the abdomen and chest. In some cases, fresh IVF cycles may result in the transfer of multiple embryos to increase the chances of successful implantation. However, this practice carries the risk of multiple pregnancies, which can have associated health risks for both the mother and the babies.
Frozen Embryo Transfer
Frozen embryo transfer, on the other hand, involves the cryopreservation of embryos for later use. These embryos are thawed and transferred into the uterus during a subsequent cycle. After the fertilization of eggs and the development of embryos in the laboratory, surplus embryos can be cryopreserved for future use. Cryopreservation involves freezing the embryos using advanced techniques to preserve their viability.
One of the primary advantages of frozen embryo transfer is the flexibility in timing. Unlike fresh cycles, FET allows for more strategic planning, enabling healthcare professionals to carefully synchronize the embryo transfer with the recipient’s menstrual cycle. FET allows for a more controlled preparation of the endometrial lining, which plays a crucial role in successful implantation. This controlled environment enhances the chances of optimal endometrial receptivity, contributing to higher success rates.
Since FET does not involve ovarian stimulation during the transfer cycle, there is no risk of ovarian hyperstimulation syndrome. This can be particularly advantageous for individuals who are prone to or have experienced OHSS in previous IVF cycles. Research and clinical evidence suggest that frozen embryo transfer may result in higher pregnancy rates compared to fresh embryo transfer. The ability to select the most viable embryos for freezing contributes to a more favorable environment for implantation.
With FET, there is a growing trend toward advocating for single embryo transfer to minimize the risk of multiple pregnancies. This approach aligns with the principles of optimizing maternal and fetal health outcomes.
Advantages of Frozen Embryo Transfer:
Research studies have indicated that frozen embryo transfer may result in higher pregnancy rates compared to fresh embryo transfer. This is attributed to the ability to select the most viable embryos for cryopreservation. FET eliminates the risk of ovarian hyperstimulation syndrome (OHSS), a potential complication associated with fresh IVF cycles. The absence of ovarian stimulation during the transfer cycle contributes to a safer reproductive process.
The flexibility in timing provided by FET allows for a more controlled preparation of the endometrial lining, promoting optimal receptivity for embryo implantation. The ability to strategically plan and time the embryo transfer in FET contributes to a more patient-friendly approach. It allows for better coordination with the patient’s schedule and the optimization of overall treatment planning.
For individuals or couples with cryopreserved embryos, FET can offer cost-effective options for pursuing additional attempts at conception without the need for a full fresh IVF cycle. For individuals or couples with embryos already cryopreserved, FET provides a means to pursue additional attempts at conception without the need for repeated ovarian stimulation and egg retrieval, minimizing waiting times between attempts.
The choice between fresh and frozen embryo transfer is a significant decision in the realm of assisted reproductive technology. Both approaches have their unique advantages and considerations, and the decision often involves a careful assessment of individual circumstances, medical history, and treatment goals. Understanding the distinctions between these methods empowers individuals and couples to make informed choices on their path toward realizing the dream of parenthood. If you want more detailed information and to be informed by doctors who are experts in their field, you can visit the official IVF website.