Sleep paralysis is a mysterious and terrifying phenomenon that affects a significant portion of the population. Those who experience sleep paralysis often wake up in the middle of the night unable to move, speak or even breathe. This can last for just a few seconds or up to several minutes, making it a truly distressing experience. Despite being a relatively common occurrence, sleep paralysis is still not entirely understood by scientists and medical professionals. However, recent research has suggested that there may be a link between genetics and sleep paralysis development. This article will explore the role of genetics in sleep paralysis and examine current research on genetic factors and mutations that may contribute to this condition.
What is Sleep Paralysis?
Have you ever woken up in the middle of the night, realizing that your body is completely paralyzed? Despite trying your best to move, you find yourself completely helpless, with a feeling of impending doom overcoming you. This strange phenomenon is known as sleep paralysis, a condition that affects millions of people around the world. Sleep paralysis is a condition that leaves you temporarily unable to move or speak while falling asleep or waking up, but what is the science behind it and what are the symptoms you need to know about? Let’s dive in and explore this mysterious condition in more detail.
The Science Behind Sleep Paralysis
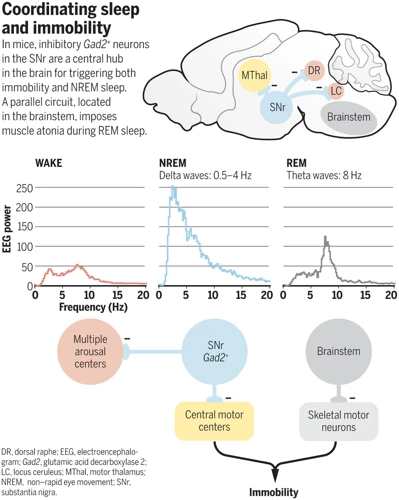
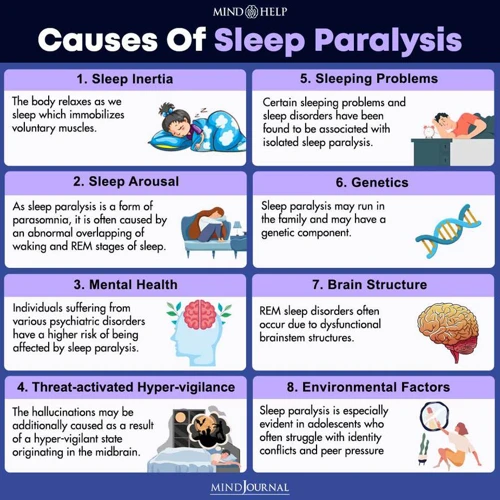
During normal sleep, the body alternates between rapid-eye-movement (REM) sleep and non-rapid-eye-movement (NREM) sleep. REM sleep is associated with vivid dreams, while NREM sleep is characterized by deep, restorative rest. Sleep paralysis occurs when the body is unable to move during the transition between these sleep cycles. The exact cause of sleep paralysis is not fully understood, but researchers have identified several factors that may contribute to its development.
Neurotransmitter Imbalance: Disruptions in the balance of neurotransmitters, such as dopamine and serotonin, may play a role in the development of sleep paralysis. These chemicals are involved in regulating sleep and wakefulness, and abnormalities in their functioning can lead to disruptions in the sleep cycle.
REM Rebound: Sleep paralysis may also be caused by a phenomenon known as REM rebound. This occurs when an individual experiences extended periods of REM sleep deprivation, such as during periods of high stress or sleep deprivation. When the individual eventually is able to enter REM sleep, they may experience an intense and prolonged REM episode, which can trigger sleep paralysis.
Brainstem Dysfunction: Sleep paralysis may also be linked to dysfunction in the brainstem, which controls many of the body’s automatic functions, such as breathing and heart rate. Abnormalities in this region of the brain may cause disruption in the sleep cycle and contribute to the development of sleep paralysis.
The underlying mechanisms of sleep paralysis are complex and not fully understood. However, by gaining a deeper understanding of the science behind this condition, researchers may be able to identify new treatments and management strategies for those who suffer from it.
Symptoms of Sleep Paralysis
Sleep paralysis is a sleep disorder that can be a terrifying experience for people who suffer from it. It is characterized by a temporary inability to move or speak while falling asleep or waking up. This phenomenon can last for a few seconds to several minutes and can be accompanied by hallucinations or delusions. Let’s explore in more detail, what are the symptoms of sleep paralysis:
| Symptoms of Sleep Paralysis |
|---|
| Inability to move: During an episode of sleep paralysis, a person may be aware of their surroundings but will be unable to move or speak. |
| Hallucinations: Sleep paralysis can be accompanied by vivid and often frightening hallucinations, which can be visual, auditory, or both. |
| Delusions: Delusions may also occur during an episode of sleep paralysis. A person may feel a sense of foreboding, or have a belief that someone or something is present in the room with them. |
| Difficulty breathing: Some people may experience a feeling of suffocation or difficulty breathing. This is because in sleep paralysis, the muscles that control breathing may also be temporarily paralyzed. |
| Rapid heartbeat: It is common to experience a rapid heartbeat during an episode of sleep paralysis. This can be a result of the fear and anxiety that the individual is experiencing. |
These symptoms can be extremely distressing, and many people who experience sleep paralysis report feeling fear, anxiety, or a sense of impending doom during an episode. It is important to remember, however, that sleep paralysis is a relatively common condition, and although it can be frightening, it is not usually a sign of a serious underlying health issue.
The Link Between Genetics and Sleep Paralysis
The mystery behind why some people experience sleep paralysis while others do not has puzzled scientists for years. However, recent studies have suggested that there may be a genetic component to this phenomenon. This is an intriguing prospect that opens up many questions about the role of genetics in sleep paralysis development. Let’s dive deeper to see what the current research is telling us.
Heritability of Sleep Paralysis
Heritability of Sleep Paralysis:
Sleep paralysis is a complex disorder that is believed to have a genetic component. In fact, studies have shown that there is a significant heritability of sleep paralysis. Here are some important points to understand about the heritability of sleep paralysis:
- Family studies: Family studies have suggested that sleep paralysis clusters within families. This means that if one family member experiences sleep paralysis, there is a higher likelihood that other family members will experience it as well.
- Twin studies: Twin studies have also suggested that there is a significant genetic factor in the development of sleep paralysis. In one study, researchers found that identical twins were more likely to both experience sleep paralysis compared to fraternal twins.
- Genetic markers: Researchers have also identified certain genetic markers that may be associated with an increased risk of sleep paralysis. For example, a mutation in the COMT gene has been linked to an increased risk of sleep paralysis, as well as other sleep disorders.
- Overall heritability: While there is still much to learn about the genetics of sleep paralysis, current research suggests that heritability plays a significant role in the development of this disorder. One study estimated that up to 60% of the variability in sleep paralysis risk can be attributed to genetic factors.
It is clear that genetics plays an important role in the development of sleep paralysis. However, as with many complex genetic disorders, there are likely multiple genes and pathways involved in the development of this condition. Further research is needed to fully understand the genetic factors contributing to the risk of sleep paralysis.
Genetic Risk Factors and Mutations
Genetic Risk Factors and Mutations
Several genetic risk factors and mutations have been identified as potential contributors to sleep paralysis. These include:
- HTR2A gene: This gene has been linked to sleep paralysis as well as other sleep disorders such as narcolepsy and REM sleep behavior disorder. The HTR2A gene encodes a protein that plays a role in the function of serotonin, a neurotransmitter that regulates sleep and mood. Mutations in this gene have been associated with an increased risk of developing sleep paralysis.
- DEFB1 gene: This gene is involved in the immune response and has been linked to the development of sleep paralysis. Mutations in this gene have been associated with an increased risk of developing sleep paralysis.
- BHLHE41 gene: This gene is involved in the regulation of the body’s internal clock or circadian rhythm. Mutations in this gene have been associated with increased levels of sleep deprivation, which can lead to sleep paralysis.
- CRY1 gene: This gene is also involved in the regulation of the body’s internal clock. Mutations in this gene have been associated with delayed sleep phase disorder, which can increase the risk of developing sleep paralysis.
While these genetic risk factors and mutations have been identified, it is important to note that not everyone with these mutations will develop sleep paralysis. Other environmental and lifestyle factors may also play a role in the development of this condition. Further research is needed to fully understand the complex interplay between genetics and other factors that contribute to sleep paralysis.
Current Research on Genetic Factors and Sleep Paralysis
Recent studies have shed light on the role of genetics in the development of sleep paralysis. The identification of genetic risk factors and mutations associated with this condition has provided valuable insights into its underlying mechanisms. In this section, we will explore the current research on genetic factors and sleep paralysis, including the significance of DEFB1 and HTR2A genes mutations in sleep paralysis development. Understanding the genetic component of this condition will be crucial in developing effective treatments and management strategies.
Mutations in DEFB1 and HTR2A genes
Current research has identified mutations in specific genes that are associated with an increased risk of developing sleep paralysis. Two of the most studied genes are DEFB1 and HTR2A.
DEFB1 is a gene that codes for a protein known as beta defensin 1, which plays a role in the immune system as an antimicrobial peptide. Several studies have found that individuals with certain variations of the DEFB1 gene are more likely to experience sleep paralysis. In one study, researchers found that individuals with a particular variation in the DEFB1 gene (rs2738047) had a significantly increased risk of developing sleep paralysis compared to those without the variation. Another study found a similar association between a different DEFB1 variation (rs1800972) and sleep paralysis.
HTR2A is another gene that has been linked to sleep paralysis development. This gene codes for a receptor protein in the brain that responds to the neurotransmitter serotonin. Some studies have found that certain variations of the HTR2A gene may increase the risk of developing sleep paralysis. For example, a study in Japanese individuals found that a specific HTR2A variation (rs6313) was associated with a higher risk of sleep paralysis.
These findings suggest that certain genetic variations may make individuals more susceptible to sleep paralysis development. The table below summarizes some of the findings on DEFB1 and HTR2A mutations and their association with sleep paralysis:
| Gene | Mutation | Association with Sleep Paralysis |
|——|———-|———————————-|
|DEFB1 | rs2738047 | Increased risk of sleep paralysis |
|DEFB1 | rs1800972 | Increased risk of sleep paralysis |
|HTR2A | rs6313 | Higher risk of sleep paralysis |
Environmental Factors and Sleep Paralysis

While genetics can play an important role in the development of sleep paralysis, it is not the only factor to consider. Environmental factors can also contribute to the onset and severity of sleep paralysis. In fact, many individuals who experience sleep paralysis report that lifestyle and environmental factors have a significant impact on their symptoms. In this section, we will explore the various environmental factors that can influence sleep paralysis and what steps you can take to manage them.
Impact of Lifestyle on Sleep Quality
The lifestyle one leads can have significant impacts on their sleep quality. This, in turn, can affect the development and severity of sleep paralysis. Here are some key lifestyle factors that can influence sleep quality:
- Stress: High levels of stress can lead to difficulty falling asleep and staying asleep. When stressed, the body produces hormones like cortisol that can interfere with our natural sleep-wake cycle. This can increase the risk of experiencing sleep paralysis.
- Diet: Eating a diet high in processed foods, sugar, and caffeine can disrupt sleep. These foods can cause blood sugar spikes, which can make it harder to fall asleep and stay asleep. Additionally, caffeine is a stimulant that can keep you awake and increase the likelihood of sleep paralysis.
- Physical Activity: Exercise can increase the quality of sleep, but doing it too close to bedtime can have the opposite effect. This is because exercise raises adrenaline levels, making it harder to wind down and fall asleep. Finding the right balance of physical activity is key.
- Sleep Environment: The environment in which you sleep can significantly influence sleep quality. A cool, dark, quiet room with comfortable bedding is ideal. Electronic devices should be kept out of the bedroom as the blue light emitted can suppress the production of melatonin, a hormone that helps regulate sleep.
Making small changes to these lifestyle factors can help improve sleep quality and potentially reduce the frequency and severity of sleep paralysis episodes.
Other Environmental Factors
Numerous environmental factors have been associated with an increased likelihood of experiencing sleep paralysis. Below is a list of some of the most influential environmental factors that have been linked to an increased risk of sleep paralysis:
- Stress: High levels of stress have been shown to increase the likelihood of experiencing sleep paralysis. Stress can disrupt sleep patterns, cause anxiety, and lead to mental health disorders – all of which can contribute to the onset of sleep paralysis.
- Sleep Deprivation: Sleep deprivation is one of the most significant environmental factors that can cause sleep paralysis. When people do not get enough sleep, their minds and bodies become exhausted, and they may experience various sleep-related disorders, including sleep paralysis.
- Substance Abuse: Substance abuse can interfere with sleep quality and can cause a wide range of sleep disorders, including sleep paralysis. Drinking alcohol, smoking cigarettes, and using drugs such as marijuana and cocaine can all exacerbate the likelihood of experiencing sleep paralysis.
- Irregular Sleep Schedule: People who have an irregular sleep schedule or who work night shifts are more likely to suffer from sleep paralysis. This is due to the fact that the human body naturally wants to sleep at night, and disrupting this natural pattern can cause issues with sleep quality.
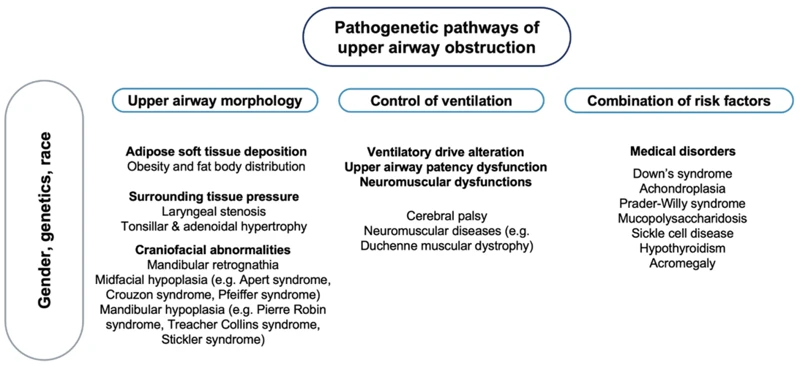
- Underlying Medical Conditions: Certain medical conditions, such as obstructive sleep apnea, narcolepsy, and psychiatric disorders, can all increase the likelihood of experiencing sleep paralysis. People with these conditions may have difficulty falling asleep or staying asleep, which can contribute to sleep paralysis.
By understanding the impact that these environmental factors can have on sleep quality and the onset of sleep paralysis, individuals can take steps to minimize their risk of experiencing this condition. Maintaining a regular sleep schedule, reducing stress, and avoiding substance abuse can all help to promote healthy sleep habits and reduce the likelihood of sleep paralysis occurring.
Treatment and Management of Sleep Paralysis
When it comes to managing and treating sleep paralysis, there’s no one-size-fits-all solution. With numerous factors that can contribute to a person’s experience with this disorder, including genetics and environmental factors, addressing sleep paralysis can be challenging. However, with proper medical treatment and lifestyle changes, people who experience sleep paralysis can find relief and improve their overall sleep quality. In this section, we will explore the various treatment options available for managing sleep paralysis and discuss potential lifestyle changes that may help alleviate symptoms.
Medical Treatments for Sleep Paralysis
Medical treatment for sleep paralysis involves addressing the underlying cause of the condition, which can vary from person to person. Here are some of the commonly used medical treatments for sleep paralysis:
| Treatment | Description |
|---|---|
| Antidepressants | These medications are often used to treat the underlying mental health conditions that can trigger sleep paralysis, such as anxiety and depression. Antidepressants can help regulate sleep cycles and reduce the frequency and intensity of sleep paralysis episodes. However, these medications are not without side effects and should be used under the close supervision of a healthcare professional. |
| Sleep aids | Prescription sleep aids such as benzodiazepines or non-benzodiazepines can be used to help regulate sleep cycles and improve the quality of sleep. However, these medications can cause dependency and should be used with caution and under the close supervision of a healthcare professional. |
| CPAP therapy | Continuous positive airway pressure (CPAP) therapy is often used to treat underlying sleep disorders such as obstructive sleep apnea, which can cause or exacerbate sleep paralysis. This therapy involves wearing a mask that delivers positive pressure to keep the airway open during sleep. |
| Medical procedures | In some cases, medical procedures such as tonsillectomies, septoplasties, or tongue reduction surgery may be recommended to treat underlying anatomical abnormalities that can cause or exacerbate sleep disorders including sleep paralysis. |
It is important to note that medical treatment for sleep paralysis should always be carried out under the close supervision of a healthcare professional. Treatment may involve a combination of medications, therapies, and lifestyle changes aimed at reducing the frequency and intensity of sleep paralysis episodes and improving overall sleep quality.
Lifestyle Changes and Self-Help Strategies
Making some simple lifestyle changes and self-help strategies can often help alleviate the symptoms of sleep paralysis. Here are some strategies that you can try:
- Improve Sleep Hygiene: Practicing good sleep hygiene such as going to bed and waking up at the same time every day, avoiding caffeine and nicotine before bedtime, and creating a comfortable sleeping environment can greatly reduce the likelihood of experiencing sleep paralysis.
- Reduce Stress: Stress can be a major trigger for sleep paralysis. Try activities such as yoga, meditation, or deep breathing exercises to reduce stress levels.
- Exercise Regularly: Regular exercise has been shown to reduce the frequency and severity of sleep paralysis episodes.
- Avoid Sleeping on Your Back: Sleeping on your back is associated with a higher risk of sleep paralysis. Try sleeping on your side instead.
- Maintain a Healthy Diet: Eating a balanced diet with lots of fruits and vegetables can help improve overall sleep quality and reduce the occurrence of sleep paralysis.
- Try Muscle Relaxation Techniques: Progressive muscle relaxation or visualization techniques can help relax your body and reduce the likelihood of sleep paralysis.
- Get Professional Help: If your sleep paralysis is affecting your daily life, consider seeking help from a therapist or sleep specialist.
By making these simple lifestyle changes and self-help strategies, you can take steps to reduce the frequency and severity of sleep paralysis episodes, and improve the quality of your sleep overall.
Conclusion
In conclusion, though the exact causes of sleep paralysis remain unknown and subject to debate, genetics seems to have a crucial role in its development. The condition appears to be heritable, with some genetic risk factors and mutations in the DEFB1 and HTR2A genes possibly contributing to its onset. However, it is important to note that environmental factors, such as lifestyle habits and stress, also play a role in sleep paralysis development.
Effective treatment and management of sleep paralysis requires a combination of medical treatments and lifestyle changes. Seeking medical advice and medication may help alleviate its symptoms, but adopting good sleep hygiene practices and reducing stress can also help prevent it.
Overall, more research is needed to understand the interplay of genetic and environmental factors involved in sleep paralysis development. As such, it is important for individuals with the condition to seek medical advice and adopt healthy habits in order to manage and live with it.
Frequently Asked Questions
What is the prevalence of sleep paralysis in the general population?
It is estimated that between 5% to 40% of the general population have experienced sleep paralysis at least once in their lifetime.
Is sleep paralysis a serious medical condition?
While sleep paralysis can be a frightening and distressing experience, it is not generally considered to be a serious medical condition.
What age does sleep paralysis usually start?
Sleep paralysis can occur at any age, but it is most commonly reported to start during adolescence or young adulthood.
Can genetics increase the risk of developing sleep paralysis?
Yes, genetics can play a role in the development of sleep paralysis through inherited risk factors and genetic mutations.
What are some common genetic risk factors for sleep paralysis?
Some common genetic risk factors for sleep paralysis include variations in the HTR2A and DEFB1 genes.
What lifestyle factors can contribute to sleep paralysis?
Poor sleep hygiene, stress, and irregular sleep patterns have been shown to increase the likelihood of experiencing sleep paralysis.
Can medication be used to treat sleep paralysis?
Yes, medication such as antidepressants and benzodiazepines may be used to treat sleep paralysis in some cases.
What self-help strategies can be used to manage sleep paralysis?
Self-help strategies for managing sleep paralysis may include improving sleep hygiene, reducing stress, and trying relaxation techniques.
How can sleep paralysis be distinguished from other sleep disorders?
Sleep paralysis is characterized by a temporary inability to move or speak while falling asleep or waking up, whereas other sleep disorders may involve different symptoms such as disrupted breathing or excessive daytime sleepiness.
Can sleep paralysis be cured?
While there is no known cure for sleep paralysis, it can often be managed through lifestyle changes and, in some cases, medical treatment.