Narcolepsy and REM sleep dysfunction are two sleep disorders that have perplexed researchers and medical professionals alike for many years. With symptoms ranging from excessive daytime sleepiness to vivid dream-like experiences during sleep, these disorders can significantly impact an individual’s quality of life. Despite much research, the root cause of these disorders remains largely unknown. In this article, we dive deeper into the connection between narcolepsy and REM sleep dysfunction, explore the common symptoms of these disorders, and discuss current methods for diagnosis and treatment.
What is Narcolepsy?
Narcolepsy is a complex and still not fully understood neurological disorder that can be perplexing for those who suffer from it, as well as for those who witness it. This disorder affects the brain’s ability to regulate sleep and wakefulness, causing sudden and uncontrollable bouts of sleepiness during the day which can severely impact daily life. At its core, narcolepsy is a disorder of the sleep-wake cycle, but its impact is much broader as it can affect cognitive function, emotional stability, and quality of life. Let’s explore this disorder in more detail and gain a deeper understanding of the mysteries surrounding it.
What is REM Sleep Dysfunction?
REM sleep dysfunction is a sleep disorder that occurs when an individual’s sleep cycle is disrupted, resulting in the loss of the normal muscle tone during REM sleep. Listed below are some characteristics of REM sleep dysfunction:
- Abnormal Muscle Movements: REM sleep dysfunction is indicated by abnormal muscle movements during sleep, such as kicking, thrashing, or punching.
- Acting Out Dreams: Individuals with REM sleep dysfunction may act out their vivid and often violent dreams during sleep.
- Arousal: Individuals with this sleep disorder may have increased heart rate, respiration, and blood pressure, accompanied by feelings of anxiety or panic.
- Disrupted Sleep Cycle: The disorder can disrupt an individual’s normal sleep cycle, leading to excessive tiredness or sleepiness during the day.
REM sleep dysfunction is more common in older adults and is linked to the development of several neurological diseases, including Parkinson’s and Alzheimer’s. It is important to seek medical attention if you believe you might be experiencing REM sleep dysfunction as it can have significant impacts on your daily life.
The Connection Between Narcolepsy and REM Sleep Dysfunction
Understanding the connection between narcolepsy and REM sleep dysfunction has puzzled researchers for decades. Despite multiple studies seeking to shed light on this complex relationship, there are still many unanswered questions. However, several promising theories have emerged in recent years, providing a glimpse into the underlying mechanisms of these conditions. In this section, we will explore the possible links between narcolepsy and REM sleep dysfunction, including the role of orexin, the impact of REM sleep behavior disorder, and other factors that may contribute to these conditions. By delving into these complex topics, we hope to gain a deeper understanding of how narcolepsy and REM sleep dysfunction are interrelated, and how this knowledge can be used to better diagnose and treat patients suffering from these conditions.
Narcolepsy and REM Sleep Behavior Disorder
Narcolepsy and REM Sleep Behavior Disorder (RBD) are two distinct sleep disorders that can occur independently or simultaneously. However, a significant association has been found between the two.
RBD is a parasomnia disorder characterized by acting out dreams during the REM sleep phase. Normally, our muscles are inhibited during REM sleep, so we don’t act out our dreams. However, in people with RBD, this inhibition is lost, leading to physical movements during REM sleep. These movements can be violent and may cause injury to the person or their sleeping partner.
Narcolepsy, on the other hand, is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. People with narcolepsy experience excessive daytime sleepiness, cataplexy (sudden muscle weakness), sleep paralysis, and hallucinations.
Studies have found that a significant proportion of narcoleptic patients also have RBD. It has been estimated that up to 30% of people with narcolepsy may experience RBD. The coexistence of the two disorders may lead to more severe symptoms and may increase the risk of injury during sleep.
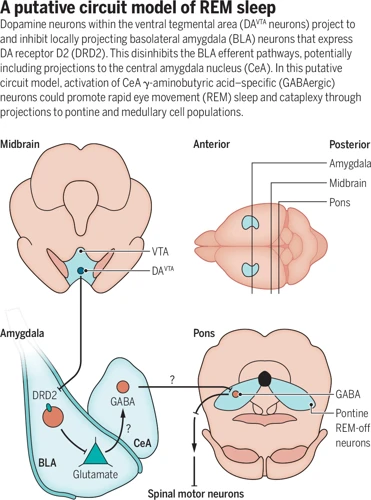
The exact relationship between narcolepsy and RBD is not fully understood, but it is thought to be related to dysfunction in the brainstem. The brainstem is responsible for regulating sleep and controlling muscle tone during sleep. Dysfunction in this area may lead to both disorders.
Treating RBD in people with narcolepsy can be challenging as the medications used to treat RBD, such as clonazepam, can worsen narcoleptic symptoms. Treatment for one disorder may exacerbate symptoms of the other disorder.
It is essential for healthcare professionals to properly diagnose and treat both disorders in individuals who experience symptoms of both narcolepsy and RBD. This treatment must be individualized and monitored carefully to minimize any potential side effects or worsening of symptoms.
How REM Sleep Dysfunction Affects Narcoleptic Sleep
One of the defining characteristics of narcolepsy is the intrusion of sleep into waking life. This can manifest as sudden and overwhelming sleepiness during the day or as periods of muscle weakness or even paralysis brought on by strong emotions. However, because narcolepsy is often comorbid with REM sleep dysfunction, individuals with the disorder also experience disruptions in their sleep cycle itself.
During the normal sleep cycle, the body cycles through periods of non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. NREM sleep is characterized by slow brainwaves and a decrease in muscle activity, while REM sleep is marked by faster brainwaves and increased muscle activity in the eyes and respiratory system. REM sleep is also the stage in which we experience most of our dreams.
REM sleep dysfunction in narcoleptic individuals can cause a number of negative sleep outcomes, including:
| Negative Sleep Outcomes of REM Sleep Dysfunction in Narcoleptics |
|---|
| Fragmented sleep: Narcoleptic individuals frequently experience interrupted sleep as a result of sudden awakenings from REM sleep. This can lead to daytime fatigue and make it difficult to perform everyday tasks. |
| Cataplexy: A symptom of narcolepsy characterized by sudden muscle weakness or paralysis brought on by strong emotions. REM sleep dysfunction can make episodes of cataplexy more likely to occur during the day. |
| Hypnagogic hallucinations: Vivid dream-like experiences that occur when falling asleep or waking up. Narcoleptic individuals with REM sleep dysfunction may experience hypnagogic hallucinations more frequently and have difficulty distinguishing them from reality. |
| Sleep paralysis: A temporary inability to move or speak that occurs when waking up or falling asleep. Narcoleptic individuals with REM sleep dysfunction may experience sleep paralysis more frequently and for longer periods of time. |
While these negative sleep outcomes can present significant challenges for individuals with narcolepsy and REM sleep dysfunction, there are effective treatments available to manage symptoms and improve overall quality of life.
The Role of Orexin in REM Sleep and Narcolepsy
Orexin is a neuropeptide that plays a crucial role in regulating wakefulness and sleep. Individuals with narcolepsy often have low levels of orexin, which can lead to excessive daytime sleepiness and other symptoms. Here are some key points about the role of orexin in REM sleep and narcolepsy:
- Orexin and Wakefulness: Orexin is produced in a small cluster of neurons in the hypothalamus, and acts on multiple brain regions to promote wakefulness. Orexin neurons are most active during the day and become less active during sleep.
- Orexin and REM Sleep: Orexin also plays a role in regulating REM sleep, which is the stage of sleep associated with dreaming. In individuals with narcolepsy, the lack of orexin can cause REM sleep to occur at inappropriate times, leading to symptoms such as hallucinations and sleep paralysis.
- Orexin and Cataplexy: One of the hallmark symptoms of narcolepsy is cataplexy, which is a sudden loss of muscle tone triggered by strong emotions. Orexin deficiency is thought to contribute to cataplexy by causing a disruption in the brain’s ability to control muscle tone.
- Orexin Receptor Agonists: Researchers have developed drugs called orexin receptor agonists, which activate the receptors that orexin would normally bind to. These drugs can help to alleviate symptoms of narcolepsy and other sleep disorders by promoting wakefulness and reducing excessive daytime sleepiness.
The role of orexin in regulating sleep and wakefulness is complex and multifaceted. A better understanding of how orexin works in the brain could lead to improved treatments for narcolepsy and other sleep disorders.
Other Factors Connecting Narcolepsy and REM Sleep Dysfunction
There are several other factors that are believed to connect narcolepsy and REM Sleep Dysfunction. Some of the key factors are:
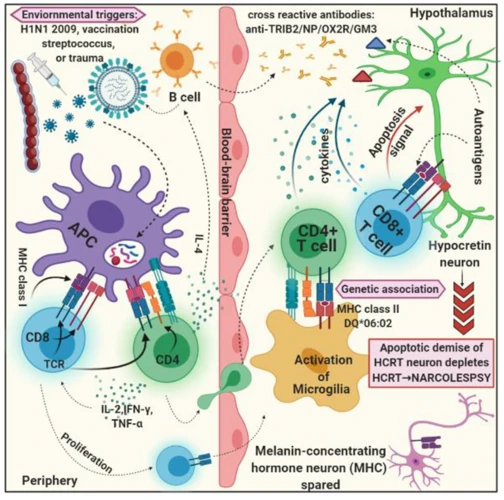
Genetic Factors: Studies have shown that narcolepsy is highly heritable, meaning that the condition can be passed down through families. Researchers have also identified certain genes, such as the HLA-DQB1 gene, that are associated with an increased risk of developing narcolepsy.
Autoimmune Response: Another factor that may be linked to both narcolepsy and REM Sleep Dysfunction is an autoimmune response. In people with narcolepsy, the immune system attacks the cells in the brain that produce orexin, a neurotransmitter that helps regulate sleep. This autoimmune response may also play a role in disrupting REM sleep.
Neurological Disorders: Some neurological disorders, such as Parkinson’s disease and multiple system atrophy, are known to cause REM Sleep Dysfunction. These disorders can also affect the same areas of the brain that are impacted in people with narcolepsy.
Stress and Trauma: Stress and trauma can also trigger narcoleptic symptoms and disrupt REM sleep. Research has shown that people with narcolepsy are more likely to experience high levels of stress and anxiety, which can worsen symptoms. Traumatic events, such as a car accident or head injury, may increase the risk of developing narcolepsy or REM Sleep Dysfunction.
Medications: Certain medications, such as antidepressants and beta-blockers, can interfere with REM sleep and may trigger narcoleptic symptoms in some people. It is important to discuss any medications you are taking with your doctor if you have narcolepsy or REM Sleep Dysfunction.
There are several possible factors that connect narcolepsy and REM Sleep Dysfunction, including genetic factors, autoimmune responses, neurological disorders, stress and trauma, and medications. Further research is needed to fully understand the complex interplay between these factors and how they contribute to the development and progression of these conditions.
The Symptoms of Narcolepsy and REM Sleep Dysfunction
It can be perplexing to differentiate the symptoms of narcolepsy and REM sleep dysfunction, as both can cause excessive daytime sleepiness and disrupted nighttime sleep. However, there are some distinct symptoms to look out for that can help identify the specific disorder. Understanding and recognizing these symptoms is crucial for receiving an accurate diagnosis and appropriate treatment. Let’s delve deeper into the common symptoms associated with these sleep disorders and how they impact your daily life.
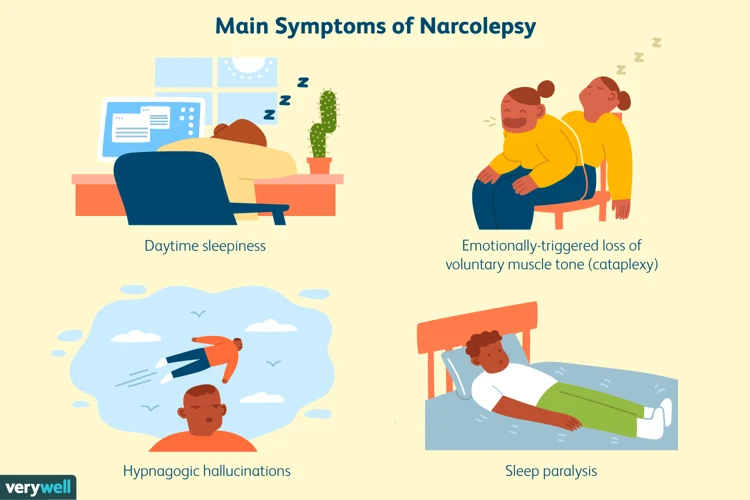
Common Symptoms of Narcolepsy
Narcolepsy is a chronic sleep disorder that is characterized by various symptoms. Some common symptoms of narcolepsy include:
- Excessive Daytime Sleepiness: People with narcolepsy feel extremely tired throughout the day, even after a full night’s sleep. They often experience sudden and uncontrollable bouts of sleepiness that can last for a few seconds to several minutes.
- Cataplexy: This is a sudden loss of muscle tone that can cause a person to collapse. Cataplexy is often triggered by intense emotions such as laughter or anger.
- Sleep Paralysis: During sleep paralysis, a person is temporarily unable to move or speak while falling asleep or waking up. This can be a frightening experience, especially if the person is unable to move or speak for several minutes.
- Hypnagogic Hallucinations: These are vivid, dream-like images that occur when a person is falling asleep or waking up. They can be very vivid and often involve senses beyond sight.
In addition to these common symptoms, people with narcolepsy may also experience disrupted nighttime sleep, automatic behavior (such as walking or talking without awareness), and difficulty concentrating or remembering things. These symptoms can significantly impact a person’s daily life, causing problems in work, personal relationships, and overall quality of life. It is important to talk to a healthcare provider if you suspect you may have narcolepsy, as treatment options are available to manage symptoms and improve quality of life.
Common Symptoms of REM Sleep Dysfunction
During REM sleep dysfunction, the person fails to experience muscle paralysis during dreams as typically occurs. As a result, there is a range of symptoms that may arise, including:
- Acting out dreams: Individuals with REM sleep disorder may act out their dreams, often resulting in injuries to themselves and/or their sleep partners.
- Vocalizations: Along with acting out dreams, individuals with REM sleep dysfunction may talk, yell, or scream during sleep.
- Jerking or twitching movements: As dreams are acted out, jerking or twitching movements in the body may occur.
- Increased heart rate and blood pressure: During episodes of REM sleep dysfunction, there may be an increase in heart rate and blood pressure, leading to potential cardiovascular complications.
- Distorted perceptions: Those experiencing REM sleep dysfunction may have distorted perceptions of their environment, resulting in confusion or disorientation when waking up from a dream.
It is important to note that while these symptoms may indicate a potential REM sleep disorder, they can also be present in other sleep disorders or medical conditions. Consulting a medical professional is essential for proper diagnosis and treatment.
How Narcolepsy and REM Sleep Dysfunction Affect Your Daily Life
Living with narcolepsy and REM sleep dysfunction can have a significant impact on a person’s daily life. Here are some ways these conditions can affect your daily life:
- Excessive daytime sleepiness: The most common symptom of narcolepsy is feeling sleepy during the day, which can make it difficult to concentrate or stay awake during work or school.
- Sudden and uncontrollable sleep: Narcoleptics may experience sleep attacks, which are sudden and uncontrollable episodes of sleep that can occur at any time during the day. These can be dangerous, especially if they happen while driving or operating machinery.
- Disrupted nighttime sleep: Narcoleptics may experience disrupted nighttime sleep due to excessive daytime sleepiness and sleep attacks during the night. This can exacerbate the symptoms of narcolepsy and make it difficult to get enough rest.
- Cataplexy: Cataplexy, a sudden loss of muscle tone, is a common symptom of narcolepsy. This can lead to falls and injuries, and may make it difficult to do physical activities.
- REM sleep behavior disorder: People with REM sleep behavior disorder may act out their dreams during sleep, which can be dangerous for themselves and their sleeping partners.
- Mood disturbances: The disruption to sleep cycles caused by narcolepsy and REM sleep dysfunction can lead to mood disturbances, including depression and anxiety.
- Social impact: These conditions may lead to social isolation and difficulties maintaining relationships due to the impact on daily life.
These challenges can be frustrating and overwhelming, but there are management strategies and treatments available to help improve quality of life for those living with narcolepsy and REM sleep dysfunction.
Diagnosing and Treating Narcolepsy and REM Sleep Dysfunction
When it comes to addressing narcolepsy and REM sleep dysfunction, a proper diagnosis is essential to begin effective treatment. However, these conditions can often be misdiagnosed or overlooked entirely, leading to years of struggle with symptoms. It’s crucial to understand the methods used to diagnose narcolepsy and REM sleep dysfunction, as well as the available treatment options. In this section, we will explore various diagnostic tools and treatment strategies, along with lifestyle changes that can help manage symptoms and improve quality of life.
Diagnosing Narcolepsy and REM Sleep Dysfunction
Diagnosing Narcolepsy and REM Sleep Dysfunction requires a thorough evaluation by a medical professional. There are several diagnostic tests that can be used to confirm a diagnosis based on specific symptoms.
|Diagnostic Test|Purpose|
|—|—|
|Polysomnography (PSG)|Monitors brain waves, heart rate, breathing, and eye movements during sleep to identify patterns and stages of sleep|
|Multiple Sleep Latency Test (MSLT)|Measures how quickly a person falls asleep during the day, and whether they enter REM sleep during these episodes|
|Hypocretin Test|Measures the level of hypocretin in cerebrospinal fluid, as decreased levels are often found in people with narcolepsy|
|Actigraphy|Wearable device that records movement and can provide information about sleep patterns and quality|
It is important for patients to provide a detailed medical history and be prepared to discuss their symptoms with their healthcare provider. This can include keeping a sleep diary or tracking episodes of sleepiness or cataplexy.
The diagnosis process may take several weeks or even months, as multiple tests may be needed to confirm a diagnosis. It is also possible for individuals to have both narcolepsy and REM Sleep Dysfunction, which can complicate the diagnosis process.
If a diagnosis is confirmed, treatment options and lifestyle changes can help manage symptoms and improve quality of life.
Treating Narcolepsy and REM Sleep Dysfunction
There are various treatment options available for managing narcolepsy and REM sleep dysfunction. Below we have listed the most common ways of treating these conditions:
1. Medications: Stimulants, such as modafinil and armodafinil, are commonly prescribed for treating excessive daytime sleepiness related to narcolepsy. Additionally, medications like sodium oxybate can help treat the symptoms of both narcolepsy and REM sleep behavior disorder.
2. Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) can help to improve nighttime sleep quality, reduce the occurrence of cataplexy, and mitigate sleep paralysis.
3. Lifestyle changes: Adopting good sleep hygiene practices such as sleeping and waking up at the same time every day, avoiding caffeine, alcohol, and nicotine before bed, and establishing a relaxing bedtime routine can significantly reduce the symptoms of narcolepsy and REM sleep dysfunction.
4. Behavioral therapies: Therapies like cognitive-behavioral therapy (CBT) can help individuals develop coping strategies and improve sleep efficiency. Additionally, practicing relaxation techniques like meditation or yoga can provide relief from sleep-related anxiety or stress.
It is important to note that treatment plans must be personalized to suit an individual’s specific needs and condition. Consulting a doctor or sleep specialist can help determine the best course of treatment.
Lifestyle Changes to Manage Symptoms
Making certain lifestyle changes can also be helpful in managing the symptoms of narcolepsy and REM sleep dysfunction. Here are some recommendations:
| Recommendation | Description |
|---|---|
| Maintain a consistent sleep schedule | Go to bed and wake up at the same time every day, including weekends. This can help regulate your body’s internal sleep-wake cycle. |
| Avoid caffeine and alcohol | These substances can interfere with sleep and exacerbate symptoms. |
| Exercise regularly | Moderate exercise can help improve energy and alertness during the day, and also promote better sleep at night. |
| Take short naps | Quick power naps (15-20 minutes) can help alleviate sleepiness and improve cognitive function without disrupting nocturnal sleep. |
| Practice good sleep hygiene | Avoid stimulating activities before bedtime, such as watching TV or using electronics. Create a comfortable sleep environment with a supportive mattress and pillows, and keep the room cool, dark, and quiet. |
Keep in mind that these lifestyle changes should be used in conjunction with other treatments, such as medication or therapy. It may also take some trial and error to find what works best for each individual in managing their symptoms.
Conclusion
In conclusion, understanding the relationship between narcolepsy and REM sleep dysfunction is crucial for effective diagnosis and treatment of these conditions. Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness, sudden muscle weakness or paralysis, and hallucinations during sleep. REM sleep dysfunction, on the other hand, is a sleep disorder that causes disruptive and often violent behaviors during sleep.
The connection between narcolepsy and REM sleep dysfunction lies in the fact that both disorders involve abnormalities in REM sleep. Narcolepsy often leads to REM sleep intrusion, which means that individuals with narcolepsy may enter REM sleep earlier than usual, sometimes even during waking hours. This can lead to symptoms such as cataplexy and sleep paralysis.
REM sleep dysfunction, on the other hand, is characterized by abnormal behaviors during REM sleep, such as sleepwalking and REM sleep behavior disorder (RBD). In RBD, individuals may act out violent or dangerous dreams during REM sleep, which can put them and their sleeping partners at risk.
Diagnosing and treating narcolepsy and REM sleep dysfunction involves a combination of medical and lifestyle interventions. Medications such as stimulants and antidepressants can help manage symptoms of narcolepsy, while medications like clonazepam and melatonin can help treat REM sleep behavior disorder. Additionally, lifestyle changes such as maintaining a regular sleep schedule, avoiding alcohol and caffeine before bedtime, and creating a comfortable sleep environment can also help manage symptoms.
Overall, by recognizing the symptoms and understanding the connection between narcolepsy and REM sleep dysfunction, individuals can seek proper diagnosis and treatment, and improve their quality of life.
Frequently Asked Questions
What causes narcolepsy and REM sleep dysfunction?
The exact cause of narcolepsy and REM sleep dysfunction is still unknown. However, research suggests that it involves a combination of genetic and environmental factors.
Is narcolepsy a rare condition?
Narcolepsy affects about 1 in every 2,000 people. It is considered a relatively rare disorder.
Can narcolepsy be cured?
There is no known cure for narcolepsy, but managing symptoms is possible with medication and lifestyle changes.
What is the most common symptom of narcolepsy?
Excessive daytime sleepiness is the most common symptom of narcolepsy. It can make it difficult to stay awake and alert during the day.
Are there any health risks associated with narcolepsy?
People with narcolepsy may be at a higher risk for accidents and injuries, especially if they fall asleep unexpectedly while driving or operating machinery.
Can REM sleep dysfunction be present without narcolepsy?
Yes, REM sleep dysfunction can occur without narcolepsy. It may be a symptom of other neurological disorders or related to medication use.
Can changing my sleep schedule help with narcolepsy?
Adjusting your sleep schedule and incorporating regular naps into your day may help manage symptoms of narcolepsy.
Are there any natural remedies for narcolepsy and REM Sleep Dysfunction?
While there is no known cure for narcolepsy or REM sleep dysfunction, some natural remedies such as exercise and a healthy diet may help improve overall sleep quality and manage symptoms.
Is it safe to drive with narcolepsy?
It can be unsafe to drive with narcolepsy, especially if you experience unexpected bouts of sleepiness or loss of muscle control. It is important to discuss driving safety with your doctor.
Can stress worsen symptoms of narcolepsy and REM sleep dysfunction?
Stress can worsen symptoms of narcolepsy and REM sleep dysfunction. Learning stress management techniques and seeking support from others can help improve overall well-being and manage symptoms.