Imagine waking up paralyzed in the middle of the night, unable to move any part of your body or even speak. The only thing you can do is stare into the darkness as terror grips you. This is the reality for people who experience sleep paralysis, a frightening condition that affects millions around the world. What’s even more baffling is the link between narcolepsy and sleep paralysis, and whether one leads to the other. In this article, we’ll take a closer look at this perplexing connection and delve into the symptoms, diagnosis, and management of both conditions.
Understanding Narcolepsy and Sleep Paralysis
Narcolepsy and Sleep Paralysis are two distinct sleep disorders that can severely impact an individual’s well-being. While both are caused by disruptions in the sleep cycle, they differ in their symptoms, triggers, and management. Narcolepsy is a chronic neurological disorder that affects the brain’s ability to regulate sleep-wake cycles, resulting in excessive daytime sleepiness and sudden uncontrollable episodes of falling asleep. On the other hand, Sleep Paralysis is a condition in which an individual is momentarily unable to move or speak upon waking up, often accompanied by vivid hallucinations. Despite their differences, Narcolepsy and Sleep Paralysis can be interlinked and understanding both disorders is crucial in developing effective treatment strategies. So, let’s delve into the details of these disorders and explore their linkages.
What is Narcolepsy?
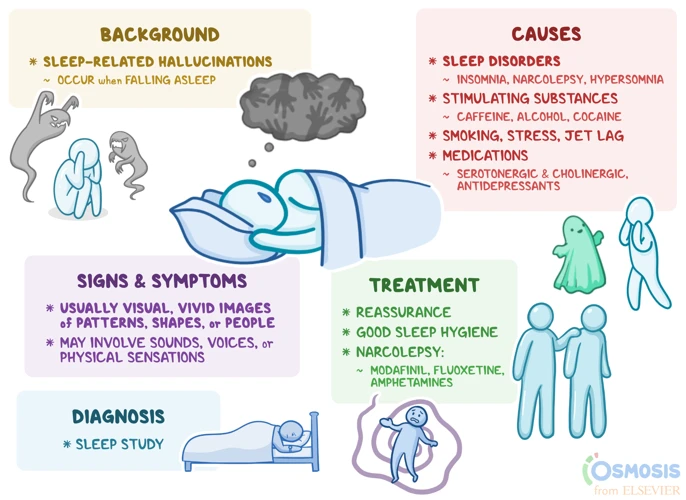
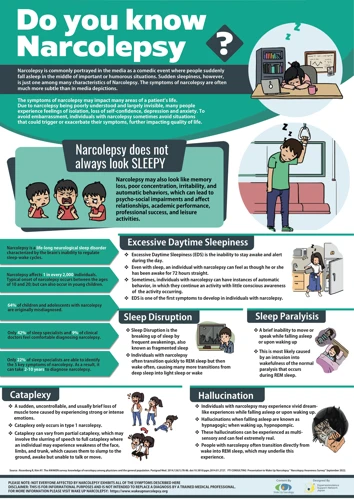
Narcolepsy is a chronic neurological disorder that affects the brain’s ability to control sleep-wake cycles. People with narcolepsy often experience involuntary episodes of sleep during the day, as well as other symptoms that can have a significant impact on their daily functioning.
Here is a table that outlines the key features of narcolepsy:
| Symptom | Description |
|---|---|
| Excessive daytime sleepiness | A persistent feeling of being tired and the need to sleep during the day, regardless of how much sleep was obtained at night. |
| Cataplexy | Sudden muscle weakness or paralysis triggered by strong emotions such as laughter, anger or excitement. |
| Hypnagogic hallucinations | Vivid or disturbing hallucinations that occur while falling asleep or waking up. |
| Sleep paralysis | A temporary inability to move or speak while falling asleep or waking up. |
Narcolepsy can be diagnosed through a sleep study, which measures brain activity and other physical signs during sleep. Treatment typically involves a combination of medications and lifestyle changes, such as sticking to a consistent sleep schedule and taking regular naps. It is important for people with narcolepsy to work with a healthcare provider to manage their symptoms and reduce the impact on their daily life.
What is Sleep Paralysis?
Sleep paralysis is a condition that causes a person to be unable to move or speak as they are falling asleep or waking up. This experience can be terrifying as the person is unable to move or speak for a short period of time, but it usually only lasts a few seconds to a few minutes. Here is a table that summarizes the main points about sleep paralysis:
| Sleep Paralysis: | Condition where a person is unable to move or speak while falling asleep or waking up |
| Durations: | Lasts a few seconds to a few minutes |
| Terrifying: | Can be a frightening experience, often accompanied by hallucinations or feeling of suffocation |
| Cause: | Disruptions in the normal sleep cycle, particularly during rapid eye movement (REM) sleep |
| Frequency: | Experienced by many people at least once in their lifetime, but frequent occurrences may signal an underlying condition such as narcolepsy |
| Treatment: | Avoidance of triggers such as stress or lack of sleep, and medications to regulate sleep patterns |
While sleep paralysis is a common experience, frequent occurrences can signal an underlying condition such as narcolepsy. It is important to speak with a healthcare provider if sleep paralysis is affecting daily life. Treatment options include avoidance of triggers such as stress or lack of sleep, as well as medication to regulate sleep patterns.
The Link Between Narcolepsy and Sleep Paralysis
The link between narcolepsy and sleep paralysis is strong, as these two conditions are often experienced together. Individuals with narcolepsy may experience sleep paralysis when their brain tries to enter REM sleep at inappropriate times, leading to an inability to move and vivid hallucinations. In fact, sleep paralysis is one of the hallmark symptoms of narcolepsy.
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, cataplexy (sudden loss of muscle control), hallucinations, and sleep paralysis. These symptoms are caused by the brain’s inability to properly regulate REM sleep, leading to an overlap between wakefulness and sleep that can occur at any time during the day.
Sleep paralysis, on the other hand, occurs when an individual is unable to move or speak during the transition between wakefulness and sleep. It is often accompanied by vivid hallucinations, and can be a frightening experience for those who have it regularly. Sleep paralysis is also a common symptom of narcolepsy, as it is typically experienced during the REM sleep cycles.
The overlap in symptoms between narcolepsy and sleep paralysis is due to the fact that they both involve disruptions in the regulation of REM sleep. In individuals with narcolepsy, the brain may enter REM sleep at inappropriate times, leading to sleep paralysis and other symptoms. Similarly, in individuals with sleep paralysis, the brain may struggle to transition out of REM sleep, leading to an inability to move and other symptoms.
Research has also found shared triggers and risk factors for narcolepsy and sleep paralysis. Both conditions have been linked to stress, anxiety, and disrupted sleep patterns. Additionally, studies have found that individuals with narcolepsy are more likely to experience sleep paralysis, and vice versa.
The link between narcolepsy and sleep paralysis is a complex and multifaceted one, with both conditions sharing many overlapping symptoms and risk factors. Understanding the connection between these two conditions is key to better managing and treating both narcolepsy and sleep paralysis.
Symptoms and Diagnosis of Narcolepsy

For those who suffer from unexplained daytime sleepiness and sudden bouts of sleep, narcolepsy may be the culprit. This chronic neurological disorder can significantly impact one’s quality of life and even lead to dangerous situations. Symptoms of narcolepsy can be frustratingly difficult to diagnose due to their seemingly unrelated nature. However, with a proper understanding of the condition, its symptoms, and diagnosis, individuals can seek appropriate treatment and lead more fulfilling lives. In this section, we’ll explore the telltale signs of narcolepsy and how it is diagnosed by medical professionals.
Symptoms of Narcolepsy
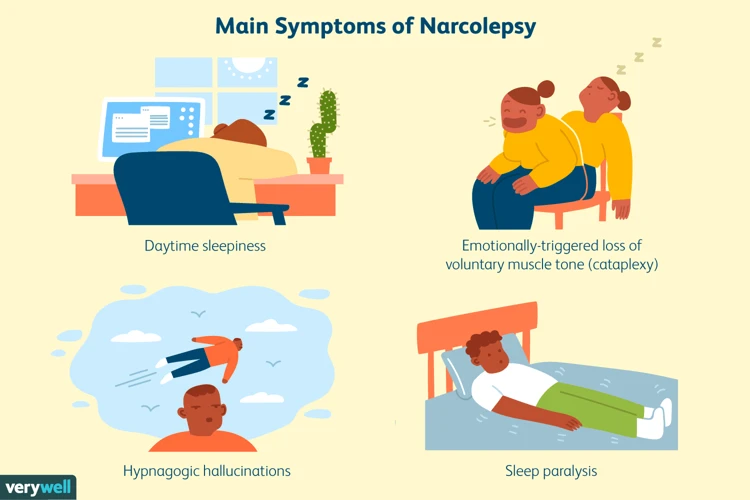
Narcolepsy is a neurological disorder that affects the sleep-wake cycle of an individual. The symptoms of narcolepsy can have a significant impact on a person’s daily life. Below are the most common symptoms experienced by individuals with narcolepsy:
- Excessive daytime sleepiness: People with narcolepsy feel an overwhelming desire to sleep during the day, making it difficult to stay awake and alert.
- Cataplexy: This is a sudden loss of muscle tone that can cause a person to feel weak or even collapse. Cataplexy is often triggered by strong emotions such as laughter or anger.
- Sleep paralysis: This happens when a person is unable to move or speak for a few seconds or minutes when waking up or falling asleep.
- Hallucinations: Individuals with narcolepsy may experience vivid and intense dream-like experiences that occur when they are falling asleep, waking up, or during the night.
- Disturbed nighttime sleep: People with narcolepsy may experience nighttime sleep disturbances such as insomnia, vivid dreams, nightmares, and frequent waking up.
- Sudden, involuntary sleep episodes: Individuals with narcolepsy may have an irresistible urge to sleep, even at inappropriate times or places, sometimes falling asleep suddenly without warning.
If you think you might have narcolepsy, it’s important to speak with your healthcare provider to get a proper diagnosis and treatment plan.
Diagnosing Narcolepsy
To diagnose narcolepsy, several diagnostic tests are required. These tests can include:
1. Sleep history evaluation: Your doctor will ask about your sleeping habits, your daytime sleepiness, and other possible symptoms of narcolepsy that you might be experiencing.
2. Sleep studies: You will be required to undergo an overnight sleep study that measures various body functions during sleep, such as brain waves, eye movements, heart rate, and breathing. This test is known as a polysomnogram.
3. Multiple sleep latency test (MSLT): This test measures how fast you fall asleep during the day. It is done during the day after an overnight sleep study. You will be asked to take four to five short naps, about two hours apart. The test measures how long it takes you to fall asleep and whether you enter rapid eye movement (REM) sleep during the day. The MSLT is considered the most reliable test for narcolepsy.
4. HLA typing: This blood test can identify certain genetic markers associated with narcolepsy.
It is vital to discuss your symptoms with your healthcare provider in detail to help determine the accuracy of a diagnosis for narcolepsy. Other conditions, such as sleep apnea or depression, can also contribute to excessive sleepiness during the day, so it is essential to rule out these conditions before concluding a diagnosis of narcolepsy.
Symptoms and Diagnosis of Sleep Paralysis
Addressing the symptoms and diagnosis of sleep paralysis is crucial for those experiencing it. This condition can be unpleasant and often frightening, and understanding its symptoms and causes is necessary for proper treatment. Sleep paralysis can be misdiagnosed as other sleep or mental disorders, making it all the more important to be aware of its diagnostic criteria. Let’s delve into the subject with a deeper understanding of the perplexing nature of sleep paralysis.
Symptoms of Sleep Paralysis
Sleep paralysis is a type of parasomnia that can affect anyone, but is most commonly experienced by people with narcolepsy. Here are some of the symptoms associated with sleep paralysis:
- Complete Muscle Weakness: During sleep paralysis, you will feel like you’re unable to move, speak or even open your eyes. This is because of complete muscle weakness that occurs during REM sleep.
- Intense Fear: Being conscious but unable to move can be an extremely frightening experience, and many people with sleep paralysis report feeling a sense of intense fear or terror.
- Hallucinations: Often, sleep paralysis is accompanied by vivid, dream-like hallucinations that can add to the feeling of fear and terror.
- Difficulty Breathing: In some cases, sleep paralysis can cause a sensation of difficulty breathing or suffocation.
- Feeling of Pressure: Some people with sleep paralysis report feeling a sensation of pressure on their chest or body, as if someone is sitting on them.
- Difficulty Sleeping: Frequent episodes of sleep paralysis can lead to difficulty falling asleep, insomnia and disrupted sleep patterns.
It’s important to note that not everyone experiences all of these symptoms during sleep paralysis, and some may have different symptoms altogether. However, if you’re experiencing any of these symptoms regularly, it’s important to talk to a doctor about your sleep health to determine if there is an underlying sleep disorder such as narcolepsy.
Diagnosing Sleep Paralysis
When it comes to diagnosing sleep paralysis, there are several factors that need to be taken into consideration by a medical professional. Sleep paralysis can be a symptom of other underlying conditions, so a thorough evaluation of a patient’s medical history and symptoms is important.
Here are some of the key factors that are considered when diagnosing sleep paralysis:
| Factor | Explanation |
|---|---|
| Medical history | A doctor will ask the patient about their history of sleep problems, including how long they have been experiencing sleep paralysis and how often it occurs. |
| Sleep study | A sleep study, also known as a polysomnography, may be ordered to monitor the patient’s sleep patterns and brain activity. |
| Physical exam | The doctor may perform a physical exam to check for any underlying causes of the sleep paralysis, such as narcolepsy or other sleep disorders. |
| Psychological evaluation | In some cases, a psychological evaluation may be necessary to rule out any underlying mental health conditions that could be contributing to the sleep paralysis. |
| Diagnostic criteria | The doctor may refer to the diagnostic criteria for sleep paralysis, which include recurrent episodes of muscle weakness or paralysis during sleep or upon waking, and the presence of hallucinations or vivid dreams that occur during an episode. |
By considering all of these factors, a medical professional can make an accurate diagnosis of sleep paralysis and develop an appropriate treatment plan for the patient. It is important for anyone experiencing symptoms of sleep paralysis to seek medical attention in order to get an accurate diagnosis and proper treatment.
The Connection Between Narcolepsy and Sleep Paralysis
As we dive deeper into the world of narcolepsy and sleep paralysis, an intriguing link arises between the two. It is not uncommon for individuals with narcolepsy to experience sleep paralysis, and vice versa. But what exactly is the connection between these two sleep disorders? Through exploring the stages of sleep and the triggers and risk factors that contribute to these conditions, we can begin to unravel the shared connections and complexities of narcolepsy and sleep paralysis.
REM Sleep and Narcolepsy
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. One of the defining features of narcolepsy is an excessive daytime sleepiness. It is also characterized by sudden and uncontrollable episodes of falling asleep during the day. These episodes can happen at any time – while at work, during meals, or even in the middle of a conversation. The symptoms of narcolepsy can severely impair a person’s ability to function in daily life.
REM sleep, or rapid eye movement sleep, is a phase of sleep characterized by heightened brain activity and vivid dreams. Normally, REM sleep occurs around 90 minutes after a person falls asleep, and it happens several times throughout the night. In people with narcolepsy, however, REM sleep can occur almost immediately upon falling asleep. This can cause intense and vivid dreams that may be difficult to distinguish from reality.
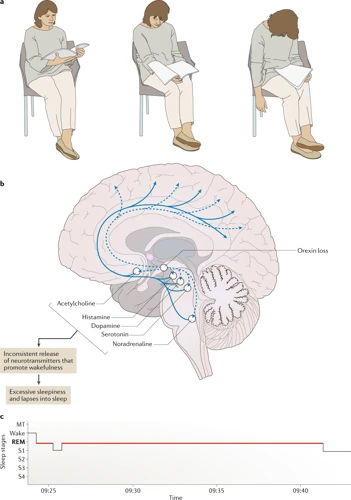
The connection between REM sleep and narcolepsy is not fully understood. However, it is believed that narcolepsy is caused by a dysfunction of the brain chemicals that regulate the sleep-wake cycle, including the neurotransmitter hypocretin. Hypocretin is important in regulating many physiological processes, including REM sleep. People with narcolepsy often have low levels of hypocretin, which may contribute to the frequent occurrence of REM sleep and the resulting symptoms of narcolepsy.
Other associated symptoms of narcolepsy include cataplexy, a sudden loss of muscle tone that can cause a person to collapse, and sleep paralysis, a temporary inability to move or speak while falling asleep or waking up.
Narcolepsy is a complex disorder that can have a profound impact on a person’s life. Understanding the relationship between narcolepsy and REM sleep is an important step in developing effective treatments for this challenging condition.
REM Sleep and Sleep Paralysis
During REM sleep, the body is in a state of paralysis, which is a normal and necessary function to prevent people from physically acting out their dreams. This is where the connection between REM sleep and sleep paralysis lies. Sleep paralysis is a condition in which an individual experiences paralysis shortly after waking up or falling asleep. This paralysis can last from a few seconds to several minutes, and during this time, the individual is unable to move or speak.
There are two types of sleep paralysis: isolated sleep paralysis and recurrent sleep paralysis. Isolated sleep paralysis occurs sporadically and is generally not a cause for alarm. Recurrent sleep paralysis, on the other hand, is a chronic condition and often indicates an underlying sleep disorder such as narcolepsy.
During episodes of sleep paralysis, individuals may also experience hallucinations or vivid dreams. These hallucinations can often be frightening and can add to the distress of the condition. However, they are a normal experience and can signal the transition in and out of REM sleep.
It’s important to differentiate between sleep paralysis and other sleep disorders, such as REM sleep behavior disorder (RBD). While sleep paralysis involves the inability to move during REM sleep, RBD involves the opposite – acting out dreams during REM sleep, often with violent or dangerous behavior. It’s essential to seek medical attention if experiencing either of these conditions to rule out any underlying conditions and to receive proper treatment.
Sleep paralysis is a unique and often frightening experience that occurs during REM sleep. While it can be a symptom of underlying sleep disorders, it can also occur in otherwise healthy individuals. Understanding the connection between REM sleep and sleep paralysis is essential in recognizing and managing this condition.
| Sleep Disorder | Definition | Key Characteristics |
|---|---|---|
| Sleep Paralysis | A condition in which an individual experiences paralysis upon waking up or falling asleep. | Paralysis, hallucinations, vivid dreams. |
| REM Sleep Behavior Disorder (RBD) | A disorder in which an individual acts out dreams during REM sleep, often with violent or dangerous behavior. | Acting out dreams during REM sleep, often with violent or dangerous behavior. |
Shared Triggers and Risk Factors
It has been observed that narcolepsy and sleep paralysis have several shared triggers and risk factors. These triggers and risk factors play a significant role in the development and occurrences of these sleep disorders. Some of the shared triggers and risk factors are listed below in the table:
| Shared Triggers | Shared Risk Factors |
|---|---|
| Stressful situations | Family history of narcolepsy or sleep disorders |
| Irregular sleep patterns | Presence of certain genes that play a role in the immune system |
| Abuse of alcohol or drugs | Autoimmune disorders such as multiple sclerosis |
| Physical trauma or injury to the head | History of infections and illnesses such as streptococcal infections and mononucleosis |
Stressful situations, irregular sleep patterns, abuse of alcohol or drugs, and physical trauma or injury to the head are the factors that can trigger both narcolepsy and sleep paralysis. Similarly, family history of narcolepsy or sleep disorders, the presence of certain genes that play a role in the immune system, autoimmune disorders such as multiple sclerosis, and history of infections and illnesses such as streptococcal infections and mononucleosis are the risk factors shared by both sleep disorders.
It is essential to recognize these shared triggers and risk factors to manage narcolepsy and sleep paralysis effectively. Avoidance of triggering situations and maintaining a regular sleep schedule can help in the management of both these disorders. Additionally, seeking medical attention in case of any physical trauma, avoiding alcohol and drug abuse, and following a healthy lifestyle can also aid in the prevention and management of both narcolepsy and sleep paralysis.
Studies Linking Narcolepsy and Sleep Paralysis
Several research studies have been conducted exploring the relationship between narcolepsy and sleep paralysis. The findings of these studies suggest a strong connection between the two conditions. One study published in the journal Sleep Medicine found that over 60% of individuals with narcolepsy experienced episodes of sleep paralysis, compared to only 15% of those without narcolepsy. Another study published in the Journal of Sleep Research found that individuals with narcolepsy were more likely to experience sleep paralysis multiple times per month and report longer episodes of paralysis compared to those without narcolepsy.
Researchers also found that sleep paralysis may be a potential diagnostic marker for narcolepsy. A study published in the Journal of Clinical Sleep Medicine found that sleep paralysis with hypnagogic hallucinations had a high positive predictive value for the diagnosis of narcolepsy with cataplexy.
Furthermore, genetic studies have shown that narcolepsy and sleep paralysis may share a genetic link. A study published in the journal Sleep Medicine Reviews found that variations in certain genes, particularly the HLA gene, are associated with both narcolepsy and sleep paralysis.
These studies provide evidence to support the link between narcolepsy and sleep paralysis. Further research is needed to fully understand the underlying mechanisms and genetic factors contributing to this connection.
| Study | Findings |
|---|---|
| Sleep Medicine (2017) | Over 60% of individuals with narcolepsy experienced episodes of sleep paralysis, compared to only 15% of those without narcolepsy. |
| Journal of Sleep Research (2011) | Individuals with narcolepsy were more likely to experience sleep paralysis multiple times per month and report longer episodes of paralysis compared to those without narcolepsy. |
| Journal of Clinical Sleep Medicine (2016) | Sleep paralysis with hypnagogic hallucinations had a high positive predictive value for the diagnosis of narcolepsy with cataplexy. |
| Sleep Medicine Reviews (2020) | Variations in certain genes, particularly the HLA gene, are associated with both narcolepsy and sleep paralysis. |
Managing Narcolepsy and Sleep Paralysis
Finding ways to manage the symptoms of both narcolepsy and sleep paralysis can be a daunting task for individuals who suffer from these sleep disorders. Treatment options can vary depending on the severity of the symptoms and the individual’s overall health. However, there are various medications and therapies that can help individuals cope with their condition and improve their quality of life. In this section, we will explore some of the current management strategies available for those affected by narcolepsy and sleep paralysis.
Medications and Therapies for Narcolepsy
Managing narcolepsy can be challenging, but there are several medications and therapies that can help alleviate the symptoms.
| Medication Name | How it Works | Possible Side Effects |
| Modafinil (Provigil) | Modafinil is a stimulant that promotes wakefulness and can improve cognitive function. | Headaches, nausea, anxiety, insomnia. |
| Armodafinil (Nuvigil) | Armodafinil is a stimulant that is similar to modafinil and can also improve wakefulness and cognitive function. | Headaches, nausea, anxiety, insomnia. |
| Sodium Oxybate (Xyrem) | Sodium oxybate is a central nervous system depressant that can improve nighttime sleep and reduce daytime sleepiness. | Nausea, dizziness, headache, confusion, depression. |
| Methylphenidate (Ritalin) | Methylphenidate is a stimulant that can promote wakefulness and improve cognitive function. It is often used in combination with other medications. | Insomnia, headaches, nausea, anxiety. |
There are also several therapies that can help manage the symptoms of narcolepsy, including:
- Cognitive-behavioral therapy – This type of therapy can help individuals develop coping strategies and improve their sleep habits.
- Nap therapy – Scheduled naps throughout the day can help reduce daytime sleepiness.
- Diet and exercise – Maintaining a healthy diet and exercise routine can help improve overall health and reduce daytime sleepiness.
- Meditation and relaxation techniques – These techniques can help reduce stress and improve sleep quality.
It is important to work with a healthcare provider to find the best treatment plan for managing narcolepsy.
Managing Sleep Paralysis
Managing sleep paralysis can be a challenging experience, but there are some strategies that can help reduce the frequency and intensity of the episodes. Here are some tips for managing sleep paralysis:
- Maintain a regular sleep schedule: Creating and sticking to a regular sleep schedule can help improve sleep quality and reduce the risk of sleep paralysis.
- Reduce stress: High levels of stress and anxiety have been linked to sleep paralysis, so finding ways to reduce stress through relaxation techniques or therapy may be beneficial.
- Avoid sleeping on your back: Sleeping on your back can increase the likelihood of experiencing sleep paralysis. Try sleeping on your side or stomach instead.
- Avoid stimulating activities before bed: Activities like watching TV, using your phone or computer, or playing video games before bed can interfere with sleep and increase the risk of sleep paralysis. Try reading a book or listening to soothing music instead.
- Practice good sleep hygiene: This includes creating a comfortable sleep environment, avoiding caffeine and alcohol before bed, and limiting daytime napping.
- Seek professional help: In some cases, treatment for underlying conditions such as narcolepsy or anxiety may help reduce the frequency and severity of sleep paralysis episodes. A healthcare professional can recommend the best course of treatment for your individual needs.
Implementing these strategies can improve your sleep quality and reduce the frequency and intensity of sleep paralysis episodes. Remember, if you experience chronic sleep paralysis or it begins to interfere with your daily life, it’s important to seek professional help.
Conclusion
In conclusion, the connection between narcolepsy and sleep paralysis is a complex and still poorly understood issue. Despite this, there are many shared risk factors and triggers between the two conditions, and researchers have discovered that they are both connected to issues with REM sleep.
The symptoms of narcolepsy and sleep paralysis can be incredibly distressing for those who experience them, and it is important to seek medical help if you suspect that you may be suffering from either condition. Fortunately, there are a variety of medications and therapies available to help manage both narcolepsy and sleep paralysis.
As research continues to delve deeper into the link between narcolepsy and sleep paralysis, we may gain a better understanding of the causes and potential treatments for these conditions. Until then, it is important to remain vigilant and seek professional help if you are experiencing symptoms of either condition.
Overall, while narcolepsy and sleep paralysis can be challenging conditions to manage, there is hope for those who suffer from them. By working with doctors and exploring various treatment options, it is possible to improve quality of life and manage the symptoms of these conditions.
Frequently Asked Questions
What is the main symptom of narcolepsy?
The main symptom of narcolepsy is excessive daytime sleepiness.
Can narcolepsy be cured?
Currently, there is no cure for narcolepsy, but the symptoms can be managed with medication and lifestyle changes.
What causes sleep paralysis?
The exact cause of sleep paralysis is not known, but it is thought to be related to the REM stage of sleep and disruptions in the normal sleep cycle.
Is sleep paralysis dangerous?
While sleep paralysis itself is not dangerous, it can be frightening and can contribute to sleep-related anxiety disorders.
How is narcolepsy diagnosed?
Narcolepsy is typically diagnosed through a combination of clinical evaluation, sleep studies, and other tests, such as the Multiple Sleep Latency Test (MSLT) and the Polysomnogram.
What is cataplexy?
Cataplexy is a sudden loss of muscle tone triggered by strong emotions, such as laughter or excitement, that is often associated with narcolepsy.
What are some triggers for sleep paralysis?
Triggers for sleep paralysis can vary from person to person but may include irregular sleep schedules, sleeping on your back, stress, and certain medications.
What is the treatment for sleep paralysis?
There is no specific treatment for sleep paralysis, but managing other sleep-related disorders, such as narcolepsy or insomnia, may help reduce the frequency of episodes.
Is there a genetic component to narcolepsy?
Yes, there appears to be a genetic component to narcolepsy, with specific genes associated with an increased risk of developing the condition.
Can lifestyle changes help manage narcolepsy?
Yes, lifestyle changes such as maintaining a regular sleep schedule, exercise, and avoiding alcohol and caffeine can help manage the symptoms of narcolepsy.