It’s no secret that sleep is vital for our survival, but what goes on in our brains during sleep remains a fascinating mystery. In particular, REM sleep has long puzzled scientists with its seemingly random and bizarre dreams. However, recent studies have shed light on the neurochemical processes that occur during REM sleep and their importance in the formation of dreams. From acetylcholine to dopamine, neurotransmitters play a crucial role in shaping our sleep experiences, and their imbalance can lead to disorders such as narcolepsy and insomnia. In this article, we’ll explore the secrets of REM sleep and its neurochemistry, and delve into the impact of hormones, stress, and medications on this mysterious stage of sleep.
Understanding REM Sleep
As we slip into slumber each night, our bodies undergo several stages of sleep, each with their own unique characteristics. One of the most fascinating and enigmatic stages is Rapid Eye Movement (REM) sleep – a time when our brain activity becomes more intense, our eyes dart back and forth, and we often experience vivid dreams. REM sleep is a complex phenomenon with many mysteries yet to be unraveled. In this section, we’ll explore the intricate world of REM sleep, delving into its definition, stages, and the fascinating neurochemical processes that underlie this phase of our sleep cycle.
Definition of REM Sleep
During sleep, there are different stages that one goes through, and REM sleep is one of them. REM stands for rapid eye movement, which is a characteristic of this stage. During REM sleep, the eyes move rapidly, and this is accompanied by a temporary paralysis of the muscles, except for the ones that control respiration and eye movement.
REM sleep is often called the dream stage because it is the stage during which most dreams occur. This stage, along with non-REM sleep, is regulated by the brain’s internal clock, which controls when we feel alert or sleepy, as well as the timing and duration of REM sleep.
REM sleep is also known as paradoxical sleep because, although the body is in a state of deep relaxation, the brain is highly active. This is because during REM sleep, there is a surge in activity in certain regions of the brain, including the amygdala and hippocampus, which are involved in the processing of emotions and memories.
During REM sleep, the body’s heart rate, blood pressure, and breathing rate increase, and there is an increase in blood flow to the brain. Additionally, there is inhibition of the neurons responsible for muscle tone, which results in the body being in a state of temporary paralysis, commonly referred to as atonia.
REM sleep usually makes up about 25% of an adult’s sleep cycle and is more frequent in babies and children. The first REM sleep period typically lasts for 10 minutes, while subsequent ones increase in duration, with the final one of the night lasting up to an hour.
Stages of REM Sleep
During REM sleep, our brain experiences rapid eye movements as well as vivid dreams. This stage of sleep is physiologically distinct from other stages of sleep and is characterized by the following stages:
- Stage 1: The onset of REM sleep usually occurs after 90 minutes of sleep. During this stage, the brain waves become more irregular, and the muscles begin to relax.
- Stage 2: In this second stage of REM sleep, the brain waves continue to become irregular, and eye movements stop. The body temperature starts to drop, and the heart rate and breathing become more irregular.
- Stage 3: This stage of REM sleep is also known as delta sleep or slow-wave sleep. During this stage, brain waves slow down significantly, and it’s much harder to wake up. It is believed that this stage is the most restorative stage of sleep.
- Stage 4: During this final stage of REM sleep, the brain becomes highly active, and the eyes move rapidly back and forth. The body is essentially paralysed to prevent movements that may occur during dreams.
These different stages of REM sleep play an essential role in the restorative process that occurs during sleep. It’s essential for individuals to experience all stages of sleep, including REM sleep, to obtain the necessary rest the body and mind need to function optimally.
Neurochemical Processes in REM Sleep
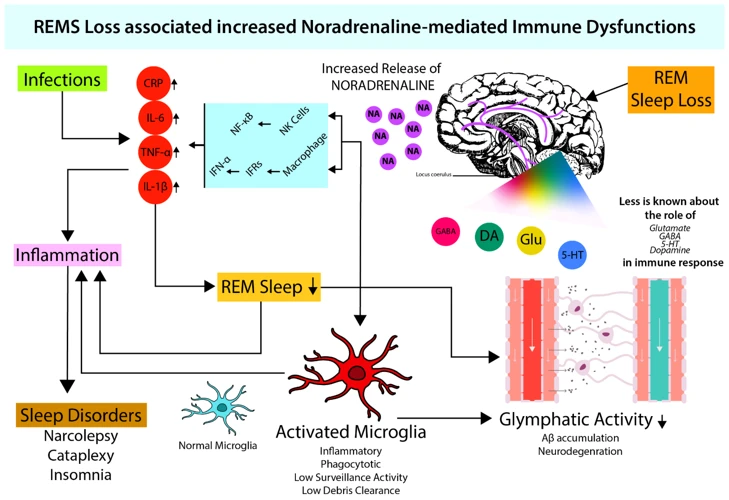
As we delve deeper into the science of sleep, the relationship between the brain’s neurochemistry and the various stages of sleep becomes increasingly intriguing. One such stage, REM sleep, is known to be associated with vivid dreams, but the exact neurochemical processes that underlie this phenomenon are not fully understood. Nonetheless, certain neurotransmitters such as acetylcholine, norepinephrine, serotonin, dopamine, GABA, and glutamate have been found to play important roles in REM sleep regulation. Let us explore the complexity of these processes and their potential implications for sleep and dream research.
Acetylcholine and Norepinephrine
Acetylcholine and norepinephrine are two neurotransmitters that play a crucial role in the neurochemistry of REM sleep. Both are involved in the regulation of the sleep-wake cycle and are important for initiating and maintaining REM sleep.
| Neurotransmitter | Function |
|———————-|————————————————————|
| Acetylcholine | Stimulates the thalamus and cortex, leading to vivid and lifelike dreams. It also inhibits motor neurons, preventing the body from acting out dreams. |
| Norepinephrine | Inhibits REM sleep, promoting wakefulness and alertness. Low levels of norepinephrine are associated with increased sleep and higher levels with decreased sleep. |
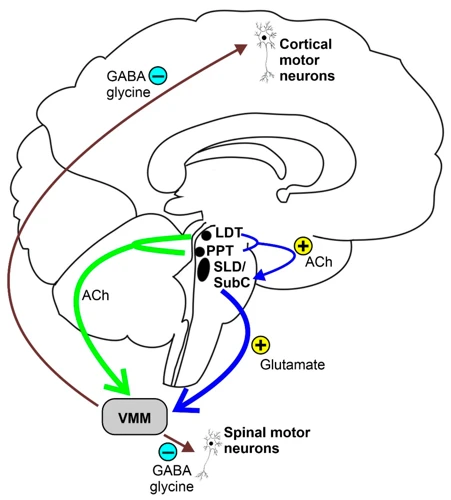
Acetylcholine is produced by neurons in the brainstem and basal forebrain and is released during REM sleep. It stimulates the thalamus and cortex, leading to vivid and lifelike dreams. Acetylcholine also inhibits motor neurons during REM sleep, preventing the body from acting out dreams, a condition known as REM sleep behavior disorder (RBD).
Norepinephrine, on the other hand, is involved in promoting wakefulness and inhibiting REM sleep. It is produced in the locus coeruleus, a group of neurons in the brainstem that become active during wakefulness and produce norepinephrine. Low levels of norepinephrine are associated with increased sleep, while higher levels are associated with decreased sleep.
The balance between acetylcholine and norepinephrine is crucial to the regulation of REM sleep. When acetylcholine levels are high and norepinephrine levels are low, REM sleep can occur. However, when norepinephrine levels are high and acetylcholine levels are low (as during wakefulness), REM sleep is inhibited.
Any imbalance in acetylcholine or norepinephrine levels, such as those seen in sleep disorders like RBD and narcolepsy, can disrupt the normal sleep-wake cycle and lead to sleep disturbances. Medications that affect these neurotransmitters can also have an impact on REM sleep and dream content.
Serotonin and Dopamine
Serotonin and dopamine are two important neurotransmitters that play a crucial role in regulating REM sleep. Serotonin is a neurotransmitter that regulates mood, appetite, and sleep. It is produced in the raphe nuclei in the brainstem and is involved in the modulation of the sleep-wake cycle. On the other hand, dopamine is a neurotransmitter that is involved in the regulation of movement, reward, and pleasure. It is produced in the substantia nigra and ventral tegmental area in the brain.
During REM sleep, the levels of these two neurotransmitters change in a specific way. Serotonin levels are at their lowest during REM sleep, while dopamine levels remain constant. This is interesting because serotonin is usually associated with calmness, while dopamine is associated with activity and arousal. This suggests that REM sleep is not as calm as we might expect.
Table:
| Neurotransmitter | Function | Location of Production | Level During REM Sleep |
|---|---|---|---|
| Serotonin | Regulation of mood, appetite, and sleep | Raphe nuclei in the brainstem | Lowest |
| Dopamine | Regulation of movement, reward, and pleasure | Substantia nigra and ventral tegmental area in the brain | Constant |
There is evidence that serotonin plays an important role in regulating the onset and duration of REM sleep. Studies have shown that reducing serotonin levels in the brain can reduce the amount of time spent in REM sleep. Similarly, increasing serotonin levels can increase the amount of time spent in REM sleep. This suggests that serotonin is involved in the initiation and maintenance of REM sleep.
Dopamine, on the other hand, appears to play a less direct role in regulating REM sleep. While dopamine levels remain constant during REM sleep, the activity of dopamine neurons changes. Specifically, dopamine neurons appear to decrease their firing rate during REM sleep. This suggests that dopamine may play a more indirect role in regulating REM sleep, possibly by modulating the activity of other neurotransmitter systems.
The interplay between serotonin and dopamine during REM sleep is complex and not yet fully understood. However, it is clear that both of these neurotransmitters play an important role in regulating REM sleep and may be involved in the generation of dream content during this stage of sleep.
GABA and Glutamate
When it comes to the neurochemical processes involved in REM sleep, two neurotransmitters that are essential are GABA and glutamate. These neurotransmitters work together in a complex interplay to regulate sleep-wake cycles, and their actions are particularly important during REM sleep.
GABA (gamma-aminobutyric acid) is an inhibitory neurotransmitter that helps to reduce the activity of neurons in the brain. It plays a critical role in promoting sleep and reducing wakefulness. GABA helps to calm the brain and nervous system, allowing the body to relax and enter a restful state.
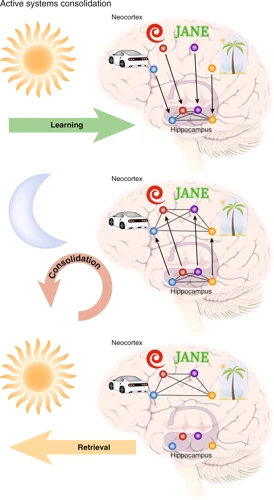
Glutamate, on the other hand, is an excitatory neurotransmitter that has the opposite effect to GABA. It increases the activity of neurons in the brain and promotes wakefulness. Glutamate is also involved in the regulation of REM sleep, and it plays an important role in the consolidation of memories.
During REM sleep, there is a delicate balance between the actions of GABA and glutamate. GABA helps to suppress the activity of neurons in the brainstem that control wakefulness, allowing the body to remain asleep. At the same time, glutamate helps to maintain the activity of neurons in the cortex, responsible for the generation of vivid dreams.
This balance between GABA and glutamate is vital, and any disruption can lead to sleep disorders or other problems. For example, if there is an excess of glutamate activity during sleep, it can lead to overstimulation and cause nightmares. Similarly, if GABA activity is impaired, it can lead to insomnia or other sleep-related issues.
GABA and glutamate are critical neurotransmitters involved in regulating sleep-wake patterns, and they play important roles during REM sleep. The balance between these neurotransmitters is essential for maintaining healthy sleep, and any disruption can lead to sleep disorders or other problems.
The Role of Neurochemistry in Dreams
As we delve deeper into the neurochemistry of sleep and its various stages, it is impossible to overlook the significant role that neurotransmitters play in shaping our dream world. Theories on dream formation have fascinated scientists for centuries, and recent research has made significant strides in understanding how neurochemical processes impact the content and vividness of our dreams. From the roles of acetylcholine and serotonin to the impact of neurochemical imbalances on sleep disorders, we explore the intricate relationship between the chemicals in our brain and the world of our dreams.
Theories on Dream Formation
One of the most intriguing aspects of REM sleep is the occurrence of vivid and often bizarre dreams. Many theories have been proposed over the years to explain the possible mechanisms behind dream formation. Here are some of the most prominent theories:
- The Activation-Synthesis Hypothesis: This theory, proposed by psychiatrist J. Allan Hobson and his colleague Robert McCarley in 1977, suggests that dreams are essentially the result of random neural activity in the brainstem and forebrain during REM sleep. According to this theory, the brainstem sends signals to the forebrain that are ultimately interpreted as a dream. This hypothesis proposes that the bizarre and often illogical nature of dreams is due to the fact that the forebrain is attempting to create meaning out of these random signals.
- The Continual-Activation Theory: This theory, proposed by sleep researcher Mark Solms in the 1990s, suggests that dreams are not randomly generated, but are instead connected to emotional and motivational systems in the brain that are activated during REM sleep. This theory suggests that dreams may be a way for the brain to process and work through emotional experiences.
- The Threat Simulation Theory: This theory, proposed by evolutionary psychologists in the early 2000s, suggests that dreams may have evolved as a means of simulating threatening situations in order to prepare the brain and body for potential danger. In this sense, dreams may serve an adaptive function by helping to improve survival and reduce risk.
- The Memory Consolidation Theory: This theory suggests that during REM sleep, the brain is able to consolidate and store memories from the previous day. Dreams may be a byproduct of this process, as the brain attempts to make sense of these newly-formed memories.
- The Psychoanalytic Theory: This theory, developed by Sigmund Freud in the late 1800s, suggests that dreams are a reflection of the unconscious mind and that they reveal hidden desires, fears, and conflicts. According to this theory, dreams serve as a kind of disguised wish-fulfillment, allowing people to act out unfulfilled desires without fear of consequences in the waking world.
While each of these theories offers a different perspective on the mechanisms behind dream formation, it is likely that a combination of factors are at play during REM sleep. The complexity of the brain and the many different systems that interact during this stage of sleep make it difficult to attribute dream formation to any one single process. Nonetheless, ongoing research continues to shed light on this fascinating aspect of the human experience.
Impact of Neurotransmitters on Dream Content
During REM sleep, the brain experiences an influx of neurotransmitters that can greatly impact the content of dreams. The table below highlights the specific effects of various neurotransmitters on dream content.
| Neurotransmitter | Effect on Dream Content |
|---|---|
| Acetylcholine | Increases visual imagery and emotional intensity of dreams |
| Serotonin | Regulates mood and can lead to more positive dream content |
| Dopamine | Increases feelings of pleasure and reward in dreams |
| GABA | Reduces dream activity and can lead to less vivid dreams |
| Glutamate | Increases brain activity during REM sleep and can lead to more complex and vivid dreams |
By understanding how these neurotransmitters affect dream content, researchers have been able to study the relationship between neurotransmitter function and the content of recurring dreams. For example, it has been suggested that people with low levels of serotonin are more likely to experience recurring nightmares.
Certain drugs that affect neurotransmitter function can profoundly impact the content of dreams. For instance, some anti-depressants that increase serotonin are known to lead to more positive dream content. On the other hand, some medications used to treat anxiety or sleep disorders that increase levels of GABA can lead to less vivid dreaming and a reduction in dream recall.
The impact of neurotransmitters on dream content is complex and multi-faceted. By studying these effects, researchers hope to develop a better understanding of the function of REM sleep and the nature of dreaming itself.
Neurochemical Imbalance and Sleep Disorders
Sleep disorders can be a cause of significant distress and impairment to an individual’s daily functioning, and they can arise from various underlying factors. One of the possible causes is the disruption in the neurochemical balance that plays a vital role in regulating the sleep-wake cycle. This disturbance can affect the quality and duration of different sleep stages, including REM sleep. In this section, we will dive into the correlation between neurochemical imbalances and some prevalent sleep disorders, their characteristics, and the possible mechanisms behind them.
REM Sleep Behavior Disorder
REM sleep behavior disorder (RBD) is a sleep disorder characterized by the loss of muscle atonia during REM sleep, causing the individual to physically act out their dreams. This disorder is more prevalent in older adults and primarily affects men. RBD is a potential precursor to neurodegenerative disorders such as Parkinson’s disease, making early diagnosis crucial.
| Symptoms of REM Sleep Behavior Disorder |
|—————————————-|
| Violent or physical movements during sleep |
| Yelling or shouting during sleep |
| Speaking or laughing during sleep |
| Acting out vivid and sometimes violent dreams |
| Thrashing, kicking or punching during sleep |
| Injury to self or bed partner during sleep |
The primary neurochemical imbalance associated with RBD is the loss of GABA and excessive activation of glutamate neurons during REM sleep. GABA is the primary inhibitory neurotransmitter in the brain and is responsible for producing muscle atonia during REM sleep. The loss of GABA leads to excessive muscle activation and physical movements during sleep.
Treatment for RBD typically involves the use of medications that increase GABA activity in the brain to restore muscle atonia during REM sleep. Clonazepam and melatonin are commonly used to treat RBD. Psychological interventions may also be beneficial in helping individuals manage the emotional and psychological effects of this disorder.
It is important to note that individuals with RBD may unknowingly cause harm to themselves or their bed partners during episodes of physical activity while asleep. Seeking medical attention for RBD is important to prevent injury and to address potential underlying neurodegenerative disorders.
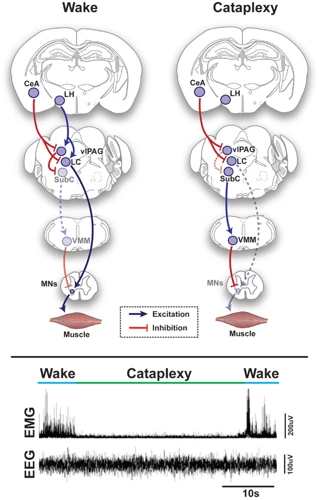
Narcolepsy
One of the most severe disorders related to REM sleep is Narcolepsy, which affects around 1 in 2,000 individuals. Narcolepsy is a neurological disorder characterized by excessive sleepiness during the day and sudden loss of muscle tone or cataplexy attacks. These attacks can be triggered by strong emotions such as laughter or excitement.
The exact cause of narcolepsy is still unknown, but researchers have found a strong association with a lack of hypocretin or orexin, a neurotransmitter involved in regulating sleep-wake cycles. Hypocretin deficiency is often caused by the loss of neurons in a specific area of the brain that produces this neurotransmitter.
Diagnosis of narcolepsy is often difficult since there are various causes of excessive daytime sleepiness. To diagnose narcolepsy, physicians typically perform a Multiple Sleep Latency Test (MSLT) which measures how quickly a person falls asleep in a quiet environment during the daytime. A sample result of MSLT is shown below in the table:
| Time After Lights Out | Stage 1 Sleep (%) | Stage 2 Sleep (%) | Stage 3 Sleep (%) | Stage REM Sleep (%) |
|---|---|---|---|---|
| Test 1 | 10 | 50 | 20 | 20 |
| Test 2 | 5 | 40 | 30 | 25 |
The MSLT result above shows that the patient has a short latency to sleep onset and a high percentage of REM sleep, which is a typical finding in narcolepsy. If narcolepsy is diagnosed, treatment usually involves medications that promote wakefulness such as modafinil or sodium oxybate, or medication to control cataplexy attacks.
If left untreated, narcolepsy can significantly impair a person’s quality of life and ability to function at work, home, or in social situations. It is essential to seek medical attention if excessive daytime sleepiness or cataplexy attacks are experienced.
Insomnia
Insomnia is a common sleep disorder that affects millions of people worldwide. It is characterized by difficulties falling asleep, staying asleep or waking up too early in the morning (1). Insomnia can be caused by a number of factors, such as stress, anxiety, poor sleep hygiene, medical conditions or medications (2). For some people, insomnia is a short-term issue that resolves on its own, while for others it can become a chronic condition that severely affects their quality of life (3).
In terms of neurochemistry, insomnia is associated with imbalances in several neurotransmitters that regulate sleep (4). Studies have shown that insomniacs have lower levels of GABA, a neurotransmitter that inhibits brain activity and promotes sleep (5). They also have higher levels of glutamate, a neurotransmitter that excites brain activity and disrupts sleep (6). These imbalances can lead to difficulties falling asleep and staying asleep throughout the night.
Insomnia is often treated with medications that target these neurotransmitter imbalances (7). For example, benzodiazepines increase the activity of GABA and promote sleep (8). Other medications, such as ramelteon and suvorexant, target other receptors that regulate sleep-wake cycles (9). However, these medications can have side effects and are not suitable for everyone. Alternative treatments, such as cognitive behavioral therapy, can also be effective in treating insomnia (10).
If you are experiencing insomnia, it is important to talk to your healthcare provider to determine the underlying cause and develop an appropriate treatment plan (11). With the right treatment, most people with insomnia can improve their sleep and regain their quality of life.
Factors Affecting REM Sleep
As with many bodily processes, the quality and quantity of REM sleep can be influenced by a variety of factors. Understanding these factors can help individuals optimize their sleep experience and potentially address any issues with sleep disorders. From hormones and age to stress and substance abuse, the influences on REM sleep are multi-faceted and can often present a perplexing challenge for people trying to achieve optimal sleep. Let’s delve into some of the factors that can affect REM sleep and explore their potential impact.
Age and Hormones
As we age, our bodies undergo various changes that affect how we sleep, including our REM sleep. Age-related changes can result in a decrease in the amount of time spent in REM sleep and an increase in the time spent in non-REM sleep, specifically stage 2.
This shift is likely caused by the decline in the production of growth hormone-releasing hormone, which naturally decreases with age. Additionally, hormonal changes in women during menopause can also impact REM sleep. Lower levels of estrogen can cause more frequent awakenings and a shorter duration of REM sleep.
Here are some of the ways age and hormones can impact REM sleep:
| Factors | Impact on REM Sleep |
|---|---|
| Aging | Decrease in amount of time spent in REM sleep |
| Menopause | Shorter duration of REM sleep |
| Low Estrogen Levels | More frequent awakenings during REM sleep |
It is important to note that not all age-related changes and hormonal changes will result in a negative impact on REM sleep. Some individuals may experience an increase in the amount of time spent in REM sleep as they age. Additionally, certain hormone replacement therapies may help improve REM sleep in menopausal women.
It is crucial to maintain a healthy lifestyle and develop proper sleep habits to ensure optimal REM sleep, regardless of age or hormonal changes.
Stress and Anxiety
Stress and anxiety have been shown to have significant effects on REM sleep. Stressful and anxiety-provoking situations can increase the amount and intensity of REM sleep. According to a study conducted by the Sleep Research Society, individuals who reported higher levels of stress during the daytime experienced significantly more REM sleep during the night.
| Effect of Stress and Anxiety on REM Sleep | Explanation |
|---|---|
| Increased REM Sleep | Stressful situations can increase the amount and intensity of REM sleep. |
| Disrupted REM Sleep | Chronic stress and anxiety can disrupt normal REM sleep patterns, leading to a decrease in overall REM sleep. |
| Nightmares | Increased levels of stress and anxiety can lead to more vivid and unpleasant dreams, including nightmares. |
This disruption of REM sleep may be due to increased levels of the stress hormone cortisol, which can inhibit REM sleep. Chronic stress and anxiety can lead to long-term changes in the brain’s neural pathways, making it more difficult to enter and sustain REM sleep. In turn, disrupted REM sleep can exacerbate feelings of stress and anxiety, creating a vicious cycle.
In order to promote healthy REM sleep, it is important to manage stress and anxiety levels. This can include regular exercise, relaxation techniques such as meditation or yoga, and seeking professional help if necessary. Certain medications may also be prescribed to help manage anxiety and promote healthy sleep patterns.
Medications and Substance Abuse
Medications and substance abuse can have a significant impact on REM sleep. Certain medications, such as antidepressants, can suppress REM sleep or delay its onset. On the other hand, medications that increase dopamine levels, such as some antipsychotics and Parkinson’s disease treatments, can cause an increase in REM sleep.
Substance abuse, particularly of alcohol and stimulants like cocaine, can also disrupt REM sleep. Alcohol may initially help a person fall asleep, but it can lead to more frequent awakenings and reduced REM sleep later in the night. Stimulants, on the other hand, can suppress REM sleep and lead to a decrease in overall sleep duration.
Additionally, withdrawal from certain substances can affect REM sleep. For example, individuals in recovery from alcohol abuse may experience “REM rebound” where they have an increase in the amount and intensity of REM sleep.
It is important to discuss any medication and substance use with a healthcare provider, as they can work with the individual to develop a plan that minimizes the impact on their sleep.
Table:
| Medications | Effect on REM Sleep |
|---|---|
| Antidepressants | Suppression or delayed onset of REM sleep |
| Antipsychotics and Parkinson’s disease treatments | Increase in REM sleep |
| Substances | Effect on REM Sleep |
|---|---|
| Alcohol | Initially helps with falling asleep, but can lead to reduced REM sleep later in the night |
| Stimulants like cocaine | Suppression of REM sleep and decreased overall sleep duration |
Conclusion
In conclusion, the study of the neurochemistry of REM sleep has been a fascinating area of research. It provides insight into the complex processes that occur in the brain during this unique stage of sleep. Acetylcholine and norepinephrine are important neurotransmitters involved in the onset and maintenance of REM sleep, while serotonin and dopamine play a role in regulating the intensity and vividness of dreams.
GABA and glutamate are also key players, modulating the overall level of neuronal activity and inhibiting certain motor functions during REM sleep. Understanding these neurochemical processes can shed light on the formation and content of dreams, as well as contribute to our knowledge of sleep disorders such as REM sleep behavior disorder, narcolepsy, and insomnia.
It is important to note that REM sleep is influenced by various factors such as age, hormones, stress, anxiety, medications, and substance abuse. For example, sleep disturbances caused by high levels of stress and anxiety can negatively impact the overall quality of REM sleep, while certain medications and substances can disrupt the balance of neurotransmitters in the brain.
Overall, more research is needed to fully understand the intricate web of neurochemical processes underlying REM sleep. However, significant progress has been made in recent years, and the potential implications of this research are vast. Advances in this field could lead to new therapies for sleep disorders, as well as a deeper understanding of the role of sleep and dreams in our overall physical and mental health.
Frequently Asked Questions
Why do we need REM sleep?
REM sleep is important for consolidating memory, regulating emotions, and restoring the brain and body. Without REM sleep, we may struggle with learning and emotional regulation.
How long does a typical REM sleep cycle last?
A typical REM sleep cycle lasts about 90-120 minutes.
What neurotransmitters are involved in REM sleep?
The neurotransmitters acetylcholine, norepinephrine, serotonin, dopamine, GABA, and glutamate all play a role in REM sleep.
Can lack of REM sleep cause health problems?
Yes, chronic lack of REM sleep can lead to a host of health problems, including cognitive deficits, mood disorders, and even an increased risk of certain diseases.
What is REM sleep behavior disorder?
REM sleep behavior disorder is a sleep disorder characterized by physically acting out dreams during REM sleep
Can stress and anxiety impact REM sleep?
Yes, stress and anxiety can interfere with REM sleep, leading to a decrease in the amount and quality of REM sleep.
Is medication the only treatment option for sleep disorders?
No, medication is not the only treatment option for sleep disorders. Other options include therapy, lifestyle changes, and alternative treatments such as acupuncture or herbal remedies.
How can substance abuse impact REM sleep?
Substance abuse, particularly of substances like alcohol and sedatives, can disrupt REM sleep and lead to sleep disorders.
Is dreaming only associated with REM sleep?
No, people can dream during any stage of sleep, but dreams are most vivid and memorable during REM sleep.
What is the role of hormones in REM sleep?
Hormones like melatonin, cortisol, and growth hormone play a role in regulating the timing and quality of REM sleep.