As we drift off into slumber, we assume that our bodies are at rest, and our minds are quiet. But for some individuals, the line between wakefulness and sleep is blurred, and they are plagued by non-REM parasomnias. These mysterious sleep disorders, encompassing night terrors and sleepwalking, have long perplexed both medical professionals and those who suffer from them. In this article, we will delve into the intricacies of non-REM parasomnias and explore their impact on individuals’ lives.
Understanding Non-REM Parasomnias
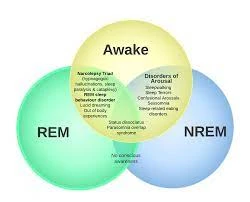
Sleep is often thought of as a peaceful, restful state of being. However, for some people, sleep can be far from tranquil. Non-REM parasomnias are a group of sleep disorders that occur during non-rapid eye movement (REM) sleep and can cause individuals to exhibit abnormal behaviors while still being asleep. Understanding non-REM parasomnias can be challenging, as they involve a complex interplay between brain activity and sleep patterns. In this section, we will explore the definition, mechanism, and brain activity behind non-REM parasomnias.
Defining Non-REM Parasomnias
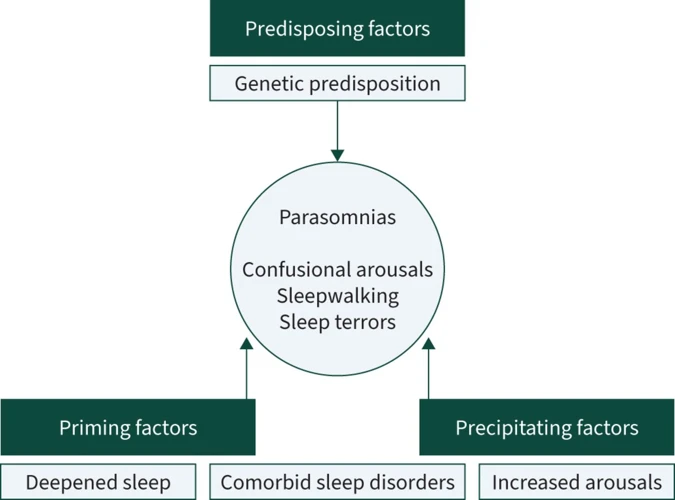
Non-REM parasomnias are a group of sleep disorders that occur during the non-rapid eye movement (NREM) sleep stage. NREM parasomnias are characterized by abnormal movements or behaviors that occur during sleep which can be detrimental to the person’s well-being.
Table: Subtypes of Non-REM Parasomnias
| Subtypes of Non-REM Parasomnias | Description |
|---|---|
| Night terrors | Intense episodes of fear and panic that occur during NREM sleep |
| Sleepwalking | Walking or performing other complex behaviors while asleep |
| Confusional arousals | Episodes of confusion and disorientation upon waking up from deep sleep |
| Sleep-related eating disorder | Eating during sleep, typically high-calorie foods |
| Sleep talking | Talking during sleep, may be coherent or incoherent |
Although many people experience non-REM parasomnias at some point in their lives, they can be a cause for concern for those experiencing frequent episodes. Night terrors and sleepwalking, in particular, can result in injuries and harm to the person experiencing the parasomnia or others around them. It’s essential to recognize the symptoms and seek professional help to manage and treat the condition.
How Non-REM Parasomnias Work
During non-REM parasomnias, the brain is in a state where it is not fully awake and not fully asleep. This can lead to behaviors that are unusual, exaggerated or beyond the control of the individual experiencing the parasomnia. Here are the steps that explain how non-REM parasomnias work:
- Stage 1 Non-REM Sleep: When a person falls asleep, they enter into stage 1 non-REM sleep. During this stage, the brainwaves slow down, and the body begins to relax.
- Stage 2 Non-REM Sleep: As the body continues to relax, the person enters stage 2 non-REM sleep. During this stage, brainwave activity slows down even further, and the body temperature drops.
- Delta Sleep: After stage 2, the body enters into delta sleep which is also known as deep sleep. During this stage, it becomes hard to wake up the person as the brainwaves are at their slowest state. The body undergoes a process of repairing tissues and rebuilding energy reserves.
- Non-REM Parasomnia: Non-REM parasomnias occur during the transition from stage 2 to delta sleep. Instead of continuing to rest and repair, the brain becomes hyperactive during this phase. The individual may suddenly sit up, walk, talk, or have a night terror, which can be upsetting or even dangerous. When someone experiences a non-REM parasomnia, they are not fully awake, but they are also not fully asleep.
Non-REM parasomnias can cause a lot of distress for the individual experiencing them. Their exact cause is not fully understood, and they can occur in anyone of any age. Learning more about the types of non-REM parasomnias and their symptoms can help people better understand their experience and seek proper treatment or management.
the Brain during Non-REM Parasomnias
During non-REM parasomnias, the activity in the brain is different from what happens during normal sleep. The movements and behaviors exhibited during these sleep disorders are thought to occur due to the conflict between different regions of the brain.
The thalamus: The thalamus is a region of the brain that filters sensory information before passing it on to other areas of the brain. During non-REM parasomnias, the thalamus is believed to be in a state of confusion, allowing sensory information to bypass this filtering system, leading to hallucinations, nightmares, and night terrors.
The amygdala: The amygdala is responsible for regulating emotions, such as fear and anxiety. During non-REM parasomnias, the amygdala may become overactive, causing intense emotions and fear during a night terror.
The frontal cortex: The frontal cortex is responsible for decision-making, problem-solving, and other executive functions. During non-REM parasomnias, the frontal cortex may not be fully awake, leading to impulsive and irrational behaviors seen in sleepwalking.
The motor cortex: The motor cortex is responsible for controlling voluntary movements. During non-REM parasomnias, the motor cortex may become active, causing movements such as sleepwalking, sleep talking, and night terrors.
The brain during non-REM parasomnias is in a unique state where different regions may be functioning differently than during normal sleep. This can lead to a variety of behaviors and movements that are unexpected and potentially dangerous. Understanding the underlying neurological mechanisms that drive these disorders is critical for developing effective treatment strategies.
The Impact of Night Terrors
Night terrors can be a perplexing and distressing experience for both the person experiencing them and those around them. These intense episodes of fear, screaming, and sudden awakening from sleep can leave individuals feeling exhausted and frightened. Although mostly affecting children, night terrors can also occur in adults and can disrupt the overall quality of sleep. In this section, we will dive into the symptoms, causes, and treatments of night terrors, as well as their impact on individual’s lives.
Symptoms of Night Terrors
Night terrors can be a perplexing phenomenon. They are not just simple nightmares. Here are some symptoms that can characterize a night terror episode:
- Intense fear or terror that wakes the person up suddenly
- Sweating, increased heart rate, and breathing difficulties
- Difficulty in arousing the person from sleep
- Rapid breathing, flailing, or thrashing
- Screaming or crying
- Confusion or disorientation
- No recollection of the event the next morning
These symptoms can be very disturbing for both the person experiencing the night terror and anyone witnessing it. It is important to note that while there are similarities between night terrors and nightmares, night terrors tend to occur during the non-REM sleep cycle, early in the night. Unlike nightmares, which occur during the later stages of sleep and typically have a narrative component, night terrors are often difficult to explain.
The Causes of Night Terrors
Night terrors, also known as sleep terrors, can be a perplexing experience for those who suffer from them. The exact cause of night terrors is not well understood, but there are some factors that may contribute to their occurrence.
Poor Sleep Habits: A lack of quality sleep, whether due to sleep deprivation, a sleep disorder, or irregular sleep schedules, can increase the likelihood of night terrors.
Stress and Anxiety: Excessive stress or heightened anxiety levels can trigger a night terror episode. This is because the body may remain in a state of hyper-arousal even during non-REM sleep, which can lead to intense, nightmarish episodes.
Genetics: Night terrors may run in families, indicating a genetic predisposition. However, more research is needed to fully understand how genetics relate to the occurrence of night terrors.
Underlying Medical Conditions: Some medical conditions such as fever, sleep apnea, restless leg syndrome, or gastroesophageal reflux disease (GERD) may trigger night terrors. Additionally, the use of certain medications, alcohol, or drugs can also increase the risk of night terrors.
It is important to note that night terrors are not caused by mental illness, despite the intense emotions and behavior that may accompany an episode. Understanding the causes of night terrors can help individuals and healthcare providers develop effective treatment plans and manage their symptoms for a better quality of life.
Treatments for Night Terrors
Night terrors can be a distressing condition for both the individual and their loved ones. However, there are several treatments available to help manage and alleviate the symptoms.
Medication: In severe cases, doctors may prescribe medication such as benzodiazepines or antidepressants to reduce the frequency and intensity of night terrors. However, they should only be used under strict medical supervision.
Talking Therapy: Night terrors can sometimes be linked to underlying psychological or emotional issues, and talking therapy can help address these root causes. Cognitive behavioral therapy (CBT) can be particularly effective in managing night terrors.
Lifestyle Changes: Small lifestyle changes can also make a big difference in managing night terrors. Creating a relaxing bedtime routine, avoiding caffeine and alcohol before bed, and ensuring a comfortable sleep environment can all help to reduce the likelihood of night terrors.
Sleep Hygiene: Good sleep hygiene is also important in managing night terrors. This means sticking to a regular sleep schedule, avoiding screens before bed, and creating a comfortable sleep environment.
It’s important to remember that treatment for night terrors will vary for each individual, and what works for one person may not work for another. Seeking professional help and advice is always recommended, especially if the night terrors are becoming frequent and disruptive to daily life.
Insight on Sleepwalking

As the night falls and we slip into slumber, some of us might encounter a peculiar phenomenon known as sleepwalking. It is a type of non-REM parasomnia that affects a small percentage of the population, yet its causes and triggers are still shrouded in mystery. In this section, we will delve into the intricacies of sleepwalking, exploring its symptoms, root causes, and available treatments. So, let us begin our voyage into the enigmatic world of sleepwalking.
The Symptoms of Sleepwalking
Sleepwalking, also known as somnambulism, is a type of non-REM parasomnia that occurs typically during the first few hours of sleep. It can be alarming for both the sleepwalker and anyone who discovers them walking around seemingly asleep. Some common symptoms of sleepwalking are:
- Moving Around: Sleepwalkers typically engage in activities that involve moving around such as walking, sitting up, or performing routine activities such as changing clothes or opening cupboards. They may look like they are awake, but they are not conscious of their actions.
- Difficulty in Awakening: Sleepwalkers don’t usually wake up easily when they are sleepwalking. They may be confused or disoriented when they do wake up, and may have little or no memory of what happened during the episode.
- Unresponsive: During a sleepwalking episode, a sleepwalker may not respond to attempts to communicate with them or wake them up.
- Blank Stare: Sleepwalkers often have a blank stare on their face as they move about, and their movements may be slower or more deliberate than when they are awake.
- Injury during Sleepwalking: Sleepwalkers may engage in dangerous activities such as leaving the house, falling down the stairs or opening a window, which can cause physical injury.
It is important to note that sleepwalking is not simply walking around in one’s sleep. It is a complex sleep disorder that requires medical attention. If you suspect that you or someone you know may be sleepwalking, it is important to consult with a healthcare provider for a proper diagnosis and treatment plan.
The Causes of Sleepwalking
Possible response:
Sleepwalking, also known as somnambulism, is a non-REM parasomnia characterized by complex motor activity during sleep. While the exact causes of sleepwalking are not fully understood, research has identified several factors that may contribute to the development and expression of this condition. Here are some of the possible causes of sleepwalking:
- Genetics: Sleepwalking seems to run in families and may have a genetic component. Studies have found that up to 80% of children with sleepwalking have at least one close relative who also sleepwalks.
- Immature nervous system: Sleepwalking is more common in children and tends to decrease in frequency and intensity with age. It is believed that sleepwalking may arise from a mismatch between the developing brain and the demands of deep sleep, which normally restricts movement.
- Medical conditions: Sleepwalking may be associated with certain medical conditions, such as sleep apnea, restless leg syndrome, and nocturnal seizures. These conditions can disrupt the quality of sleep and trigger abnormal sleep behaviors.
- Stress and anxiety: Sleepwalking may be triggered or exacerbated by emotional stress, anxiety, or trauma. These factors can affect the regulation of sleep and wakefulness and increase the likelihood of sleep disturbances.
- Medications and substances: Sleepwalking may be a side effect of certain medications, such as sedatives, hypnotics, and antidepressants. Alcohol and drugs can also alter the brain’s chemistry and impair the quality of sleep, which may lead to sleepwalking.
- Environmental factors: Sleepwalking can be triggered by environmental stimuli, such as noise, light, temperature, or physical contact. For example, a loud noise or a bright light may disrupt sleep and cause a sleepwalking episode.
While these factors may contribute to the development of sleepwalking, not everyone who experiences them will necessarily sleepwalk. The exact triggers and mechanisms of sleepwalking remain a subject of ongoing research, and more studies are needed to understand this intriguing behavior.
Treatments for Sleepwalking
Sleepwalking or somnambulism can be a perplexing condition not only for the person affected but also for the caregivers. Although sleepwalking often resolves on its own, there are some treatments available that can help to reduce its occurrence and severity. Here are some of the treatments for sleepwalking:
- Creating a safe sleeping environment: People who sleepwalk should sleep on the ground floor or even in a room on the first floor if possible. Locking doors and windows and blocking the stairs can also prevent the person from wandering out of the house while sleepwalking.
- Implementing a regular sleep schedule: Ensuring that the person gets enough sleep and follows a consistent sleep schedule can reduce the occurrence of sleepwalking.
- Reducing stress: Stress can trigger sleepwalking. Relaxation techniques, such as meditation or yoga, can help to manage stress.
- Avoiding alcohol and sedatives: Alcohol and sedatives can trigger sleepwalking or make it worse, so it is essential to avoid these substances.
- Medications: In some cases, doctors may prescribe medication to reduce sleepwalking episodes. Hypnotic medications, such as benzodiazepines or antidepressants, can help to improve sleep quality and reduce the frequency of sleepwalking.
It is essential to seek medical attention if sleepwalking is frequent, severe, or poses a risk to the person’s safety. A healthcare professional may recommend a treatment plan or refer the person to a specialist who can advise on the best management approach.
Prevention and Management
As we delve deeper into understanding non-REM parasomnias like sleepwalking and night terrors, we must also explore ways to prevent and manage them. While there is no surefire way to completely eradicate these parasomnias, there are measures that can be taken to lessen their impact on our daily lives. It is a perplexing situation when we find ourselves in the midst of a non-REM parasomnia episode and the fear of the unknown can be overwhelming. However, with the right knowledge and tools, managing these parasomnias becomes more achievable. Let us explore some techniques and lifestyle changes that can aid in the prevention and management of non-REM parasomnias.
Managing Sleepwalking and Night Terrors
Managing Sleepwalking and Night Terrors can be challenging, but there are several strategies individuals can adopt to help prevent and manage these non-REM parasomnias.
Establish a regular sleep routine: Going to bed and waking up at consistent times can help regulate sleep patterns and reduce the likelihood of sleepwalking and night terrors.
Create a safe sleeping environment: Keep the bedroom free of clutter and hazards that could cause injury during an episode. Additionally, locking doors or installing alarms can help prevent sleepwalking episodes from resulting in dangerous situations.
Avoid stress and anxiety triggers: Managing stress and anxiety through relaxation techniques like meditation or yoga can reduce the frequency of non-REM parasomnias. Avoiding stimulants like caffeine or sugary foods before bed can also help calm the mind and reduce the likelihood of an episode.
Speak with a physician: A medical professional can assess an individual’s overall health and help create a personalized treatment plan. They may also recommend medication, therapy, or other interventions to manage sleepwalking or night terrors.
Consider a sleep study: If episodes are frequent or severe, a sleep study can help identify potential underlying issues like sleep apnea or restless leg syndrome that may be contributing to the non-REM parasomnia.
Involve family and roommates: It can be helpful to inform family members or roommates about an individual’s sleepwalking or night terror episodes so they can assist in managing the situation and ensuring safety.
By adopting these strategies, individuals can reduce the frequency and severity of sleepwalking and night terror episodes, and better manage this unique sleep disorder.
Lifestyle Changes to Prevent Non-REM Parasomnias
There are several lifestyle changes that can help prevent non-REM parasomnias such as sleepwalking and night terrors. Here are some tips to consider:
- Establish a consistent sleep schedule by going to bed and waking up at the same time every day. This will help your body get into a natural sleep rhythm and minimize the risk of disturbances.
- Avoid caffeine and alcohol before bedtime. Both substances can interfere with your sleep quality and increase the likelihood of experiencing non-REM parasomnias.
- Try to minimize stress and anxiety through relaxation techniques such as meditation, deep breathing, or yoga.
- Make sure your sleep environment is comfortable and safe. Keep your bedroom dark, quiet, cool, and comfortable. Also, remove any objects that could cause harm if you were to sleepwalk or experience a night terror.
- Avoid watching television or using electronic devices in bed. The blue light emitted by screens can suppress the release of melatonin, making it harder to fall asleep and increasing the risk of non-REM parasomnias.
By implementing these lifestyle changes, you can improve your sleep quality and reduce the likelihood of experiencing non-REM parasomnias. If you still find yourself struggling with sleepwalking or night terrors, it may be time to seek professional help.
Seeking Professional Help
If you or someone you know is experiencing non-REM parasomnias such as sleepwalking or night terrors, it is important to seek professional help. While lifestyle changes and self-management techniques can be helpful, professional guidance can ensure that the condition is properly diagnosed and treated.
Medical Evaluation: A medical evaluation is the first step in seeking professional help for non-REM parasomnias. A doctor can conduct a physical examination, as well as run tests and analysis to rule out any underlying medical conditions. They may also recommend a Sleep Study or Polysomnography – a non-invasive test that records brain waves, blood oxygen levels, and other body functions while sleeping.
Psychological Evaluation: In some cases, psychological evaluation may also be necessary. Mental disorders or stress can trigger sleepwalking or night terrors. Therapy or counseling can help deal with these underlying issues.
Treatment Options: A doctor can recommend various treatment options, depending on the severity and frequency of the non-REM parasomnias. These can range from medication and therapy to supervised awakenings and even surgery in rare cases.
It is important to note that non-REM parasomnias can have serious impacts on daily life, including increased fatigue, anxiety, and stress. If left untreated, these conditions can lead to physical harm or injury. Seeking professional help is crucial to managing and treating non-REM parasomnias effectively.
Conclusion
In conclusion, non-REM parasomnias, such as sleepwalking and night terrors, can be frightening and disruptive to the individual and their loved ones. While they may appear mysterious and difficult to understand, there is a growing body of research that sheds light on how these phenomena occur and can be managed.
It is important for individuals to seek professional help if they consistently experience non-REM parasomnias, as they can be a sign of an underlying sleep disorder or other health condition. In addition, lifestyle changes can often make a big difference in preventing and managing these sleep disturbances.
It’s also important to emphasize that family members of those experiencing non-REM parasomnias should not judge or blame the individual for their behaviors, as this can exacerbate the problem and lead to increased stress and anxiety. Instead, taking a compassionate and proactive approach to dealing with non-REM parasomnias can greatly benefit both the individual and their loved ones.
Overall, while non-REM parasomnias may seem mysterious and scary, there are many effective ways to prevent and manage these sleep disturbances. With the right combination of lifestyle changes and professional support, individuals with non-REM parasomnias can achieve a restful and rejuvenating night’s sleep, free from disruptive behaviors and frightening experiences.
Frequently Asked Questions
What are some potential triggers of night terrors?
Potential triggers of night terrors include sleep deprivation, stress, certain medications, and substance abuse.
Can sleepwalking cause harm?
Yes, sleepwalking can cause harm. It’s important to create a safe sleeping environment to prevent injuries.
What is the difference between night terrors and nightmares?
Night terrors occur during non-REM sleep and typically involve intense fear and physical symptoms, whereas nightmares occur during REM sleep and are more vivid, story-like dreams.
Is there a genetic component to non-REM parasomnias?
Yes, there may be a genetic component to non-REM parasomnias. Studies have shown a potential link between certain genetic variations and an increased risk of sleepwalking and night terrors.
Can medication be used to treat non-REM parasomnias?
Medication can be used to treat non-REM parasomnias in some cases, but it’s important to consult with a healthcare professional before starting any treatment.
Can caffeine consumption worsen non-REM parasomnias?
Yes, consuming caffeine can worsen non-REM parasomnias by disrupting sleep quality and increasing arousal during the night.
Is it possible to prevent night terrors?
While it may not be possible to completely prevent night terrors, promoting good sleep hygiene and managing stress can help reduce the likelihood of experiencing them.
Are non-REM parasomnias more common in children or adults?
Non-REM parasomnias are more common in children, but can still occur in adults.
Can sleepwalking be dangerous for others besides the sleepwalker?
Yes, sleepwalking can be dangerous for others if the sleepwalker accidentally harms them.
Are there certain mental health conditions that are associated with non-REM parasomnias?
Yes, certain mental health conditions, such as anxiety and depression, have been associated with an increased risk of experiencing non-REM parasomnias.