Have you ever woken up feeling irritable, groggy, and unable to concentrate? Sleep is essential for our physical and mental well-being, and inadequate sleep can have detrimental effects on our health. Researchers have discovered that different stages of sleep play a crucial role in maintaining our mental health. In particular, non-REM sleep, the stage of sleep without rapid eye movement, has been found to impact various aspects of mental health, including memory consolidation, emotional regulation, and the development of psychiatric disorders. In this article, we will explore the relationship between non-REM sleep and mental health, learn about the factors that affect non-REM sleep quality, and discover ways to improve our sleep hygiene.
Exploring Non-REM Sleep
Have you ever wondered about the different stages of sleep your body goes through each night? One of these stages is non-REM sleep, which accounts for around 75% of your total sleep time. While it may not be as well-known as the popular REM sleep, non-REM sleep plays a crucial role in your physical and mental health. In this section of the article, we’ll delve deeper into what non-REM sleep actually is, the various stages involved, and why it’s so essential for your well-being.
What is Non-REM Sleep?
Non-REM sleep, or NREM, is a type of sleep that occurs during the first half of the night. It is characterized by low levels of brain activity and slower brainwaves compared to REM sleep. In this stage of sleep, the body is in a state of relaxation, and the muscles are not active. The heart rate and breathing slow down, and the body temperature drops.
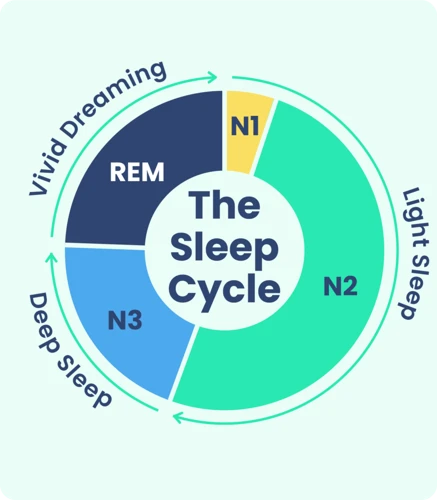
There are three stages of non-REM sleep, each characterized by different brainwave patterns. They are as follows:
| Stage | Description | Brainwaves |
|---|---|---|
| Stage 1 | Also known as light sleep, this stage typically lasts a few minutes. It is characterized by drowsiness and relaxation of the muscles. | Alpha and Theta waves |
| Stage 2 | In this stage, the brainwave activity slows down even further. The body temperature drops, and the heart rate and breathing become more regular. | Theta waves with sudden bursts of sleep spindles and K-complexes |
| Stage 3 | Also known as deep sleep, this stage is the deepest and most restorative stage of sleep. The brainwave activity is at its slowest, and the muscles are completely relaxed. | Delta waves |
Non-REM sleep is different from rapid-eye-movement (REM) sleep, which is a later stage of sleep. During REM sleep, the brain is highly active, and the muscles are paralyzed. REM sleep is when most memorable dreams occur.
Both types of sleep are necessary for overall well-being, and lack of NREM or REM sleep can lead to physical, cognitive, and emotional impairment.
Stages of Non-REM Sleep
Non-REM sleep is the stage of sleep that is characterized by a slower brain wave activity and reduced muscle tone. It is divided into three stages, which are based on the level of brain activity and other physiological changes:
- Stage 1: This is the transition stage between being awake and asleep. The brain produces alpha and theta waves, and the body starts to relax. This stage lasts only a few minutes.
- Stage 2: This stage is characterized by a further reduction in brain activity and the onset of sleep spindles – brief bursts of brain activity that last between 0.5-2 seconds. Breathing and heart rate further slow down, and body temperature drops.
- Stage 3: This is the deepest and the most restorative stage of non-REM sleep. Also known as slow-wave sleep (SWS), this stage is characterized by delta waves – the slowest and longest brain waves. It is during this stage that the body repairs and regenerates tissues, boosts the immune system, and consolidates memories.
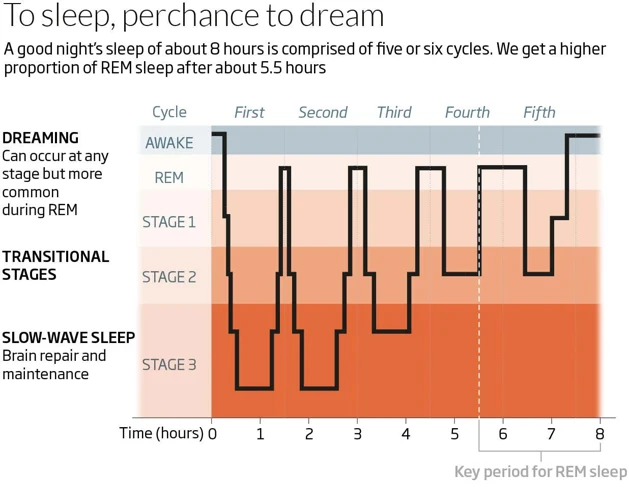
The stages of non-REM sleep progress in a cycle, with each cycle lasting about 90 minutes, and repeating several times throughout the night. The proportion of each stage varies depending on the age and sleep needs of an individual. For instance, children and teenagers tend to spend more time in SWS than adults, while older individuals experience less deep sleep.
Why is Non-REM Sleep Important?
Non-REM sleep is a crucial part of our sleep cycle, and its importance cannot be overstated. Below are some of the reasons why non-REM sleep is essential for our physical and mental health:
- Cell restoration: During non-REM sleep, our body undergoes a process of cell restoration and repair. This is because the growth hormone is released, which helps in repairing and regenerating tissues, muscles, and bones.
- Energy conservation: Non-REM sleep is responsible for the conservation of energy. During this sleep cycle, our body’s metabolic rate slows down, leading to a decreased energy expenditure. This decrease in energy expenditure allows us to conserve energy and feel more refreshed.
- Cognitive restoration: Our brain also gets the much-needed rest and restoration during non-REM sleep. It is responsible for cognitive restoration and is critical in memory consolidation, learning, and general brain functioning.
- Regulating hormones: Non-REM sleep is also important in regulating hormones in our body. This includes hormones related to appetite, stress, and growth.
- Immune system functioning: Non-REM sleep also plays a vital role in enhancing the functioning of our immune system. This is because cytokines are released, which are instrumental in protecting us from infections, inflammation, and other diseases.
Non-REM sleep is a significant part of our overall sleep cycle, and its proper functioning is vital in maintaining good physical and mental health. A lack of non-REM sleep can lead to several health problems such as memory deficits, impaired cognitive functioning, and an increased risk of psychiatric disorders.
The Connection Between Non-REM Sleep and Mental Health
As we delve deeper into the world of sleep, we cannot ignore the link between non-REM sleep and mental health. Studies have shown that non-REM sleep plays a crucial role in maintaining mental well-being and any disruption to this phase of sleep can have negative repercussions on our emotional state. In this section, we will explore the connection between non-REM sleep and mental health, and how it can impact our memory, emotions and psychiatric well-being.
Sleep Disorders and Mental Health
Sleep disorders are common and can be linked to various mental health conditions. Insomnia, sleep apnea, restless leg syndrome, and narcolepsy are some of the most commonly known sleep disorders. Insomnia, in particular, has been linked to anxiety and depression. Those with insomnia have trouble falling or staying asleep, leading to irritability, fatigue, and difficulty concentrating during the day.
Sleep apnea, on the other hand, can lead to decreased oxygen supply to the brain and increased risk of stroke and cardiovascular disease. It is also linked to depression and anxiety. Restless leg syndrome causes an uncomfortable sensation in the legs and an urge to move them, leading to sleep disruption and increased risk of depression and anxiety. Narcolepsy, which causes excessive daytime sleepiness, has been linked to depression and anxiety disorders, as well as an increased risk of accidents due to falling asleep during the day.
It’s important to note that sleep disorders and mental health conditions can affect each other in a cyclical manner. Poor sleep can lead to worsening mental health conditions, which in turn can lead to worsening sleep. Addressing both the mental health condition and the sleep disorder is important for overall physical and mental health.
Non-REM Sleep and Memory Consolidation
During non-REM sleep, our brain processes and consolidates information from our day, including memories. This is essential for better learning and memory retention. Here are some key points about the link between non-REM sleep and memory consolidation:
- Memory consolidation: Non-REM sleep plays a crucial role in memory consolidation, which is the process of transforming short-term memories into long-term memories. During non-REM sleep, the brain replays and strengthens memories acquired during the day.
- Types of memory: The two types of memories that non-REM sleep helps consolidate are declarative memory (facts and events) and procedural memory (skills and habits).
- Slow-wave activity: Slow-wave activity, which is a characteristic of non-REM sleep, has been linked to memory consolidation. Studies have shown that high levels of slow-wave activity during non-REM sleep are associated with better memory performance.
- Sleep spindles: Sleep spindles are brief bursts of electrical activity that occur during non-REM sleep. They have been found to play a role in memory consolidation, specifically in relation to declarative memory.
- Disruptions to memory consolidation: Disruptions to non-REM sleep, such as sleep deprivation or sleep disorders, can impair memory consolidation and lead to forgetfulness and difficulty learning.
Non-REM sleep is essential for memory consolidation and better learning. Ensuring adequate quality and quantity of non-REM sleep is crucial for optimal cognitive functioning.
Non-REM Sleep and Emotional Regulation
During Non-REM sleep, emotional regulation occurs in the brain. This is because the amygdala, which is responsible for processing emotions such as fear and anxiety, essentially “talks” to the prefrontal cortex, which regulates our emotional responses. This communication between these brain regions is essential for healthy emotional regulation.
Studies have shown that individuals who experience disrupted Non-REM sleep have a greater difficulty regulating their emotions. Disrupted sleep can lead to increased levels of negative emotions, as well as a decreased ability to regulate them.
One study found that people who were kept awake all night had increased emotional reactivity when viewing negative images, as opposed to people who had a good night’s sleep. The study also found that individuals who experienced poor-quality sleep had a greater likelihood of developing symptoms of depression.
It is important to note that this relationship between Non-REM sleep and emotional regulation is bidirectional. Poor emotional regulation can also lead to disrupted sleep, which in turn exacerbates emotional dysregulation.
It is crucial to prioritize good sleep habits and regulate our emotions, especially if we struggle with psychiatric disorders or chronic stress. Practicing stress-reduction techniques, seeking therapy, and implementing good sleep hygiene practices can all help to promote healthy Non-REM sleep and emotional regulation.
Non-REM Sleep and Psychiatric Disorders
Studies have found a strong link between Non-REM sleep and various psychiatric disorders. Let’s have a closer look at them:
| Psychiatric Disorders | Non-REM Sleep Abnormalities |
|---|---|
| Depression | Reduced slow wave sleep (SWS) and sleep continuity disturbances |
| Bipolar Disorder | Abnormalities in SWS, increased REM density and reduced latency to non-REM sleep |
| Anxiety Disorders | Reduced SWS and hyperarousal during sleep |
| Schizophrenia | Reduced SWS and abnormal sleep architecture |
It is important to note that sleep disturbances are not only a common symptom but also a risk factor for developing various mental health problems. Individuals with insomnia are particularly at risk for developing depression, anxiety, and substance abuse disorders. Any treatment plan for psychiatric disorders should also address sleep issues to improve overall outcomes.
Factors that Affect Non-REM Sleep Quality
As we discussed earlier, non-REM sleep plays a crucial role in maintaining our mental and physical health. However, various factors can impact the quality and duration of non-REM sleep. It is imperative to identify these factors and take appropriate measures to improve the quality of our sleep. In this section, we will explore some of the lifestyle factors, medical conditions, medications, and substance abuse issues that can affect non-REM sleep quality. Let’s delve into the details and understand how each of these factors affects our sleep patterns.
Lifestyle Factors
Various lifestyle factors can significantly affect the quality of non-REM sleep. These factors include diet, exercise, caffeine consumption, and bedtime routines.
| Lifestyle Factors | Influence on Non-REM Sleep |
|—|—|
| Diet | Consuming heavy meals or foods high in sugar or fat close to bedtime can interfere with sleep quality. |
| Exercise | Regular exercise can improve sleep quality and promote deep, restorative sleep. However, exercising close to bedtime can stimulate the body and disrupt sleep. |
| Caffeine Consumption | Consuming caffeine, a stimulant, close to bedtime can disrupt sleep quality and reduce the amount of deep sleep achieved during the night. |
| Bedtime Routines | Having a consistent bedtime routine can help signal the body when it is time to sleep, promoting healthy sleep habits. However, engaging in stimulating activities such as watching TV or using electronic devices before bed can inhibit sleep. |
It’s important to note that everyone’s biology and lifestyle habits are different, and what works for one person may not work for another. Making conscious efforts to develop healthy sleep habits and finding a routine that works best for individuals can optimize non-REM sleep and ultimately lead to better overall mental health.
Medical Conditions
Various medical conditions can also affect the quality of non-REM sleep. Here are some examples:
| Medical Condition | Description |
|---|---|
| Obstructive Sleep Apnea | Individuals with this condition experience abnormal breathing during sleep, which causes frequent interruptions throughout the night, leading to poor sleep quality and reduced non-REM sleep. |
| Fibromyalgia | People with this chronic pain disorder often have difficulty falling asleep and staying asleep, and may experience non-refreshing sleep. As a result, they may spend less time in non-REM sleep. |
| Parkinson’s Disease | Individuals with Parkinson’s disease may experience disrupted sleep patterns, including reduced non-REM sleep, due to the degeneration of nerve cells in the brain. |
| Chronic Pain | Individuals with chronic pain may have difficulty falling asleep and staying asleep, and may experience reduced non-REM sleep as a result of the pain and discomfort. |
| Depression | Depression is associated with alterations in sleep patterns, including reduced non-REM sleep, which may further exacerbate symptoms of depression. |
| Anxiety Disorders | Individuals with anxiety disorders may experience difficulty falling asleep and staying asleep, which can lead to reduced non-REM sleep and further contribute to anxiety symptoms. |
It is important for individuals with these medical conditions to work with their healthcare provider to receive appropriate treatment for their condition, which may help improve their non-REM sleep quality.
Medications and Substance Abuse
Numerous medications and substances may impact the quality of Non-REM sleep. Here are some of the most common ones:
- Stimulants: Taking stimulants such as caffeine, nicotine, or energy drinks can lead to difficulty falling asleep, staying asleep, and achieving deep sleep. The effects of stimulants can last up to 12 hours.
- Depressants: Depressants such as alcohol and sedatives can help people fall asleep faster, but they interfere with deep sleep, which is crucial for cognitive functioning and memory consolidation. Chronic use of these substances can lead to long-term sleep problems.
- Antidepressants: Some antidepressants may have sedative effects and improve sleep, but others can lead to insomnia or fragmented sleep. It’s important to talk to your healthcare provider about the side effects of any medications you’re taking.
- Antipsychotics: Antipsychotics can lead to daytime sleepiness, weight gain, and other side effects, which can interfere with sleep. They should only be prescribed by a licensed healthcare professional for specific mental health conditions.
- Pain medications: Pain medications such as opioids can interfere with sleep by causing shallow breathing, night sweats, and frequent awakenings.
- Recreational drugs and substances: The use of recreational drugs and substances such as marijuana, cocaine, and methamphetamine can interfere with sleep by causing insomnia, vivid dreams, and other side effects.
It’s important to talk to your healthcare provider about any medications you’re taking and to avoid the use of recreational drugs and substances to promote the quality of Non-REM sleep.
Ways to Improve Non-REM Sleep
Getting enough non-REM sleep is crucial for maintaining optimal mental health and overall wellbeing. However, various factors such as lifestyle habits, medical conditions, and medication use can disrupt this type of sleep, leading to negative consequences for mental and physical health. Fortunately, there are several effective methods for improving non-REM sleep quality. In this section, we will explore some of the most effective techniques and strategies backed by science to help you get better sleep and feel more energized and refreshed upon waking up. From adopting good sleep hygiene practices to using medication and other therapies, there are several options to choose from depending on your individual needs and preferences. Let’s dive in and explore everything you need to know about improving your non-REM sleep!
Sleep Hygiene Practices
One of the best ways to improve the quality of your Non-REM sleep is to practice good sleep hygiene. Sleep hygiene refers to the practices and habits that are conducive to quality sleep. Here are some examples of sleep hygiene practices that can help improve Non-REM sleep:
- Establish a consistent sleep schedule. Going to bed and waking up at the same time every day (even on weekends) can help regulate your sleep-wake cycle and promote more consistent Non-REM sleep.
- Create a relaxing bedtime routine. Engage in activities that help you wind down before bed, such as taking a warm bath, reading a book, or practicing relaxation techniques like deep breathing or progressive muscle relaxation.
- Create a sleep-conducive environment. Your sleep environment should be quiet, dark, and cool in order to promote Non-REM sleep. Consider using earplugs, an eye mask, or a white noise machine to minimize disruptions.
- Avoid stimulating activities before bed. Activities like watching TV, using electronic devices, or doing work can interfere with your ability to fall asleep and experience deep Non-REM sleep.
- Avoid consuming stimulants and alcohol before bed. Caffeine, nicotine, and alcohol can all disrupt Non-REM sleep, so it’s best to avoid consuming them close to bedtime.
- Exercise regularly. Regular physical activity can help improve the quality of your sleep, but it’s best to avoid exercising too close to bedtime, as it can be too stimulating.
By practicing good sleep hygiene, you can help optimize your Non-REM sleep and improve overall sleep quality. These practices can be especially helpful for individuals with sleep disorders, such as insomnia or sleep apnea, which can interfere with the amount and quality of Non-REM sleep they experience.
Cognitive Behavioral Therapy for Insomnia (CBTI)
CBTI, or Cognitive Behavioral Therapy for Insomnia, is a type of psychotherapy that focuses on identifying and changing negative thought patterns and behaviors that contribute to insomnia. It is considered the gold standard treatment for chronic insomnia and can help improve outcomes for individuals with a range of psychiatric disorders.
CBTI typically involves several components, including education about sleep and insomnia, stimulus control therapy, sleep restriction therapy, relaxation training, and cognitive therapy.
The education component helps individuals understand the link between thoughts and behaviors and their effects on sleep, while stimulus control therapy focuses on creating a strong association between the bed and sleep. Sleep restriction therapy restricts the amount of time spent in bed to the amount of time actually spent sleeping to improve sleep efficiency, while relaxation training helps individuals learn techniques to reduce physical and mental tension.
Lastly, cognitive therapy focuses on identifying and challenging negative thought patterns related to sleep and insomnia. It helps individuals change irrational beliefs and develop positive coping strategies to manage insomnia.
CBTI has been shown to be an effective treatment for insomnia both on its own and in combination with medication. It is a recommended first-line treatment for chronic insomnia and has been shown to improve sleep quality and duration, reduce time to fall asleep, and reduce waking up during the night.
| CBTI components | Description |
|---|---|
| Education | Helps individuals understand the link between thoughts and behaviors and their effects on sleep. |
| Stimulus control therapy | Focuses on creating a strong association between the bed and sleep. |
| Sleep restriction therapy | Restricts the amount of time spent in bed to the amount of time actually spent sleeping to improve sleep efficiency. |
| Relaxation training | Helps individuals learn techniques to reduce physical and mental tension. |
| Cognitive therapy | Focuses on identifying and challenging negative thought patterns related to sleep and insomnia. |
Medications and Other Therapies
There are several medications and therapies available for improving non-REM sleep. Here are some of the most commonly used ones:
- Sleep aids: Prescription sleep aids like zolpidem and eszopiclone can help improve non-REM sleep, but they should be used cautiously and under a doctor’s supervision to avoid adverse effects.
- Antidepressants: Some antidepressants, such as trazodone, can also improve non-REM sleep. However, they should be used only for treating depression and not solely for improving sleep.
- Antianxiety medications: Benzodiazepines and other antianxiety medications can help with sleep, but they can also cause dependence and withdrawal symptoms if used long-term. They should be used with caution and only for a short period of time.
- Light therapy: Exposure to bright light in the morning can help regulate the body’s sleep-wake cycle, which can improve non-REM sleep at night.
- Relaxation techniques: Techniques like meditation, yoga, and deep breathing exercises can help reduce stress and promote relaxation, which can in turn improve non-REM sleep.
- Exercise: Regular exercise can help improve overall sleep quality, including non-REM sleep.
It is important to note that medication and other therapies should not be the first line of treatment for improving non-REM sleep. Sleep hygiene practices and non-pharmacological interventions like cognitive behavioral therapy for insomnia (CBTI) should be tried first. Consult with a healthcare professional for more information on the best course of treatment for your specific sleep needs.
Conclusion
As we come to the end of our exploration of the link between non-REM sleep and mental health, it is clear that there is a complex relationship between the two. The science shows us that non-REM sleep is crucial for maintaining good mental health, as it plays a role in memory consolidation, emotional regulation, and may offer protective effects against certain psychiatric disorders. However, we have also seen that there are many factors that can affect non-REM sleep quality, including lifestyle factors, medical conditions, medications, and substance abuse. Despite these challenges, there are also a variety of ways to improve non-REM sleep, including sleep hygiene practices, cognitive behavioral therapy for insomnia, and other therapies. Overall, the importance of non-REM sleep for mental health cannot be overstated, and it is something that we must all strive to prioritize in our daily lives.
Summary of the Article
This article explored the link between non-REM sleep and mental health. It described what non-REM sleep is, the stages of non-REM sleep, and why it is important. The article then delved into the connection between non-REM sleep and mental health, outlining the relationship between sleep disorders and mental health, the role of non-REM sleep in memory consolidation and emotional regulation, and the impact of non-REM sleep on various psychiatric disorders.
The article also discussed factors that affect non-REM sleep quality, including lifestyle factors, medical conditions, and medications or substance abuse. The article provided ways to improve non-REM sleep, such as sleep hygiene practices, cognitive behavioral therapy for insomnia (CBTI), and various medications and therapies.
This article highlights the crucial role that non-REM sleep plays in maintaining good mental health, and offers insights and solutions for individuals looking to improve their quality of sleep and mental well-being.
Final Thoughts
Final Thoughts
The link between non-REM sleep and mental health is undeniable. Non-REM sleep plays a crucial role in various mental health aspects, such as memory consolidation, emotional regulation, and the development of psychiatric disorders.
It is imperative to understand the factors that affect non-REM sleep quality, as they can have detrimental effects on mental health. Lifestyle factors, such as smoking, excessive alcohol consumption, and lack of exercise, can disrupt the quality of non-REM sleep.
Medical conditions and medications can also have a significant impact on the quality of non-REM sleep. It is crucial to speak with a healthcare professional if you have a medical condition that affects your sleep quality or if you are taking medication that interferes with sleep.
Fortunately, there are ways to improve non-REM sleep quality. Sleep hygiene practices, such as avoiding caffeine and having a consistent sleep schedule, can have positive effects on sleep quality. Cognitive Behavioral Therapy for Insomnia (CBTI) is a form of therapy that has shown promising results in treating sleep-related issues.
In some cases, medication and other therapies may be necessary to improve non-REM sleep quality. It is essential to discuss these options with a healthcare professional before starting any treatment.
Prioritizing non-REM sleep and taking steps to improve its quality can have significant benefits for mental health. Good sleep hygiene and seeking professional guidance can be powerful tools in achieving better sleep and ultimately better mental health.
Frequently Asked Questions
What is the recommended amount of Non-REM sleep for adults?
Most adults need between 7 and 9 hours of sleep per night, including several cycles of Non-REM sleep.
Can lifestyle factors such as diet affect Non-REM sleep?
Yes, a diet high in processed foods and sugar can interfere with Non-REM sleep, whereas a diet high in fiber and whole foods can improve sleep quality.
What are some common medical conditions that can affect Non-REM sleep?
Medical conditions such as sleep apnea, restless leg syndrome, and chronic pain can all interfere with Non-REM sleep.
Can taking certain medications affect Non-REM sleep?
Yes, medications such as antidepressants, beta blockers, and certain allergy medications can interfere with Non-REM sleep.
What is the role of Non-REM sleep in memory consolidation?
During Non-REM sleep, the brain consolidates memories and information learned during the day, which is essential for optimal cognitive functioning and learning.
Can lack of Non-REM sleep contribute to the development of psychiatric disorders?
Research suggests that chronic lack of Non-REM sleep may contribute to the development of psychiatric disorders such as depression and anxiety.
What is Cognitive Behavioral Therapy for Insomnia (CBTI)?
CBTI is a form of therapy that helps individuals restructure negative thought patterns and behaviors related to sleep, allowing for improved sleep quality.
Are there any natural remedies or supplements that can improve Non-REM sleep?
Natural remedies such as melatonin and valerian root may improve sleep quality, but it is important to consult with a healthcare professional before starting any new supplements.
Can alcohol consumption negatively affect Non-REM sleep?
Yes, while alcohol may initially help with falling asleep, it can disrupt the later stages of Non-REM sleep, leading to decreased sleep quality and next-day cognitive impairment.
Is it possible to improve Non-REM sleep without medication?
Yes, practicing good sleep hygiene, engaging in relaxation techniques such as meditation or deep breathing, and avoiding electronic devices before bed can all improve Non-REM sleep without medication.