Sleep is an essential part of our daily lives, allowing our bodies and minds to rest and rejuvenate. However, for many people, sleep is not a peaceful and restful experience. Rather it can be a constant battle against various sleep disorders that can disrupt the normal sleep process. One of the most critical stages of sleep is Rapid Eye Movement (REM) sleep. The disruption of REM sleep can lead to significant health issues and decreased quality of life. It is important to understand the role that sleep disorders can play in disrupting REM sleep and how treatment options can help alleviate these issues. So let’s delve deeper into this topic and explore how sleep disorders can impact REM sleep.
What is REM Sleep?

One of the most important stages of sleep is REM (Rapid Eye Movement) sleep, which is characterized by rapid eye movements, increased brain activity, and vivid dreaming. During REM sleep, the body is in a state of muscle paralysis, and the eyes move rapidly back and forth, while the brain is highly active.
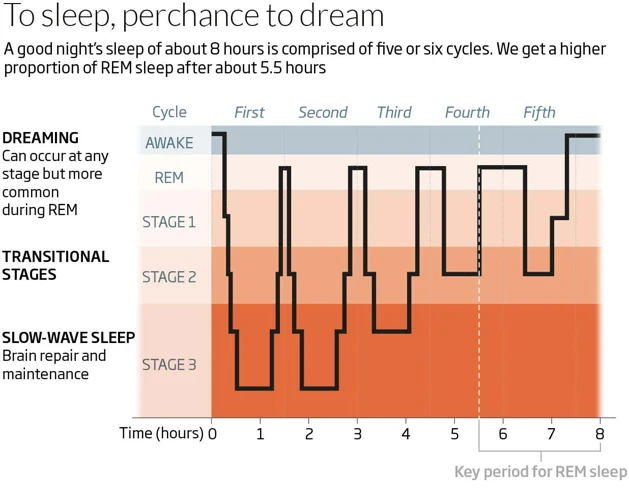
The Stages of Sleep are divided into four distinct stages, each characterized by unique patterns of brain activity and physiological changes. Stage 1 sleep is the lightest form of sleep and is characterized by a falling sensation and muscle twitching. In contrast, stage 2 sleep is deeper and represents about 50% of the total sleep time in adults. Stages 3 and 4 are considered deep sleep, also known as slow-wave sleep, which is essential for physical restoration.
The Importance of REM Sleep is vital for cognitive functions such as learning, memory consolidation, and emotional regulation. REM sleep helps strengthen memories and connects them with prior knowledge and experiences. Additionally, rapid eye movements may help stimulate the visual cortex and improve visual memory.
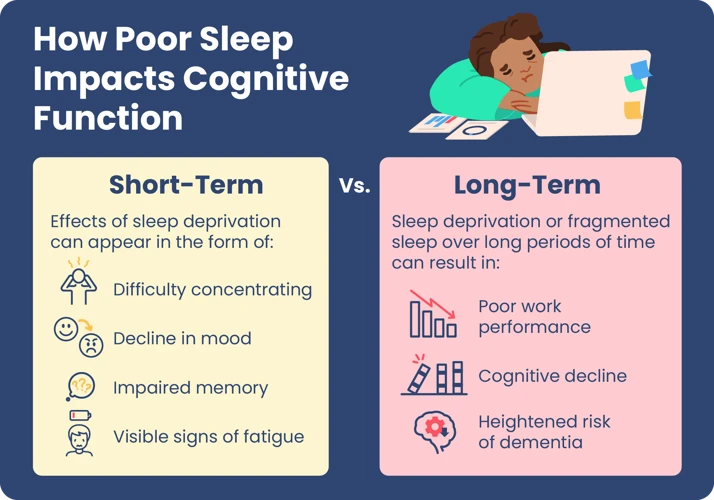
REM sleep is essential for maintaining optimal cognitive and emotional functioning, and its disruption can lead to a range of negative consequences, including mood disturbances and impaired cognitive performance.
The Stages of Sleep
Sleep is a complex physiological process that involves different stages. During the night, our body goes through a cycle of four distinct stages of sleep, which are classified into two types: non-REM (NREM) sleep and REM sleep.
NREM Sleep: NREM sleep is the first stage of sleep and accounts for about 75% of our total sleep time. It is further divided into three stages: stage 1, stage 2, and stage 3. During stage 1, which is the lightest stage of sleep, we drift in and out of sleep and can be easily awakened. Our brain produces alpha and theta waves, which are slower than the beta waves produced when we are awake.
REM Sleep: REM sleep, which stands for rapid eye movement, is the fourth stage of sleep and occurs about 90 minutes after we fall asleep. It is the stage of sleep where dreaming occurs, and our brain activity is similar to when we are awake. Our breathing becomes more irregular, our eyes move rapidly, and our muscles become paralyzed. REM sleep accounts for about 25% of our sleep time, and it occurs several times throughout the night, becoming longer in duration as the night progresses.
The cycle of NREM and REM sleep is repeated several times during a typical night’s sleep. The first complete sleep cycle lasts approximately 90 minutes, with NREM sleep occurring in the first half and REM sleep occurring in the second half. As the night progresses, the amount of time spent in REM sleep increases, while the amount of time spent in NREM sleep decreases.
Each stage of sleep plays a crucial role in allowing our body to rest and recover. The different stages of sleep are important for different physiological and cognitive functions, and any disruption to this cycle can lead to sleep disorders and other health problems.
The Importance of REM Sleep
During the course of a good night’s sleep, a healthy sleeper progresses through various stages of sleep, with each stage serving its own purposes. Rapid eye movement (REM) sleep is a crucial stage of sleep that has many important functions. REM sleep is characterized by rapid eye movements, muscle paralysis, and vivid dreaming.
One of the primary functions of REM sleep is memory consolidation. During this stage, the brain forms new connections between neurons and consolidates memories from the previous day. This process is important for learning and memory and can help individuals better retain information from their waking hours.
REM sleep is also important for emotional regulation. Studies have shown that people who get less REM sleep are more likely to experience anxiety, depression, and other emotional disturbances. REM sleep allows the brain to process and regulate emotions, which is essential for overall mental health.
REM sleep plays a role in physical health as well. During this stage of sleep, the body produces growth hormone, which is necessary for healthy development and repair of cells, tissues, and muscles. Additionally, a lack of REM sleep has been linked to increased risk of obesity, diabetes, and other health problems.
REM sleep is a crucial stage of sleep that serves many important functions for overall health and well-being.
Common Sleep Disorders
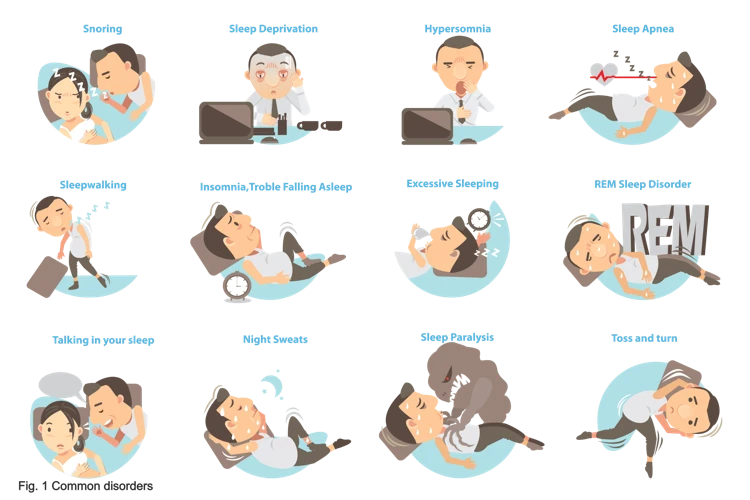
There are several sleep disorders that affect millions of people around the world. These disorders can significantly impact the quality and quantity of sleep, resulting in daytime drowsiness, fatigue, and other health problems.
Insomnia is a common sleep disorder that is characterized by difficulty falling asleep, staying asleep, or both. Approximately one-third of adults experience symptoms of insomnia, which can be caused by various factors such as stress, anxiety, depression, or environmental factors such as noise, light, or temperature.
Sleep Apnea is a sleep disorder that is characterized by recurrent episodes of partial or complete cessation of breathing during sleep. This disorder affects approximately 20 million adults in the United States alone and can lead to daytime sleepiness, fatigue, difficulty concentrating, and other health problems.
Restless Leg Syndrome is a neurological disorder that causes an irresistible urge to move the legs, especially during periods of inactivity or at bedtime. This disorder affects approximately 10% of adults and can significantly disrupt sleep and lead to daytime fatigue and other health problems.
Narcolepsy is a neurological disorder that causes excessive daytime sleepiness, sudden episodes of muscle weakness or paralysis, and vivid hallucinations during sleep. This disorder affects approximately 1 in 2,000 people and can significantly impact a person’s quality of life and daily functioning.
Insomnia
Insomnia is a common sleep disorder that affects individuals of all ages. This disorder is characterized by difficulty falling asleep, staying asleep, or waking up too early in the morning. People with insomnia often experience fatigue, irritability, and daytime sleepiness. The causes of insomnia can vary and can include environmental factors, psychological factors, medical conditions, or certain medications.
Environmental Factors: Environmental factors can include noise, light, temperature, or uncomfortable sleeping arrangements.
Psychological Factors: Psychological factors that contribute to insomnia can include stress, anxiety, depression, or other mental health conditions.
Medical Conditions: Medical conditions such as chronic pain, asthma, or gastrointestinal disorders can interfere with sleep and cause insomnia. Additionally, certain medications for these conditions may also cause insomnia as a side effect.
It is important to properly diagnose and treat insomnia as it can significantly impact an individual’s quality of life. Treatment options for insomnia may include cognitive behavioral therapy, prescription medications, or a combination of both. Cognitive behavioral therapy focuses on addressing the underlying causes of insomnia and creating healthy sleep habits. Prescription medications, such as hypnotic medications, can be used to help people fall asleep more easily, but can also come with potential side effects and should be used under a doctor’s supervision.
If insomnia is left untreated, it can have a significant impact on an individual’s overall health and well-being, including a disruption of their REM sleep. This disruption can lead to decreased cognitive function, reduced immune function, and an increased risk of developing other physical and mental health conditions.
Sleep Apnea
Sleep apnea is a common sleep disorder that affects millions of people around the world. It is a condition where a person experiences a pause in breathing while they sleep. This pause can last for a few seconds to a minute or more and can occur multiple times throughout the night.
Types of Sleep Apnea: There are two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA).
Obstructive sleep apnea: This is the most common type of sleep apnea, which occurs due to the obstruction of the airway. The airway can become narrowed or blocked when the throat muscles relax, causing snoring or gasping for breath. This type of sleep apnea is associated with obesity, smoking, and alcohol consumption.
Central sleep apnea: This type of sleep apnea is rare and occurs when the brain fails to send the proper signals to the muscles that control breathing. CSA is often associated with underlying medical conditions such as cardiovascular diseases or neurologic disorders.
Symptoms of Sleep Apnea: The most common symptom of sleep apnea is snoring. However, not all people who snore have sleep apnea. Other symptoms of sleep apnea include daytime sleepiness, morning headaches, dry mouth or sore throat upon waking up, difficulty concentrating, and irritability or mood changes.
Impact of Sleep Apnea on REM Sleep: Sleep apnea can disrupt REM sleep by causing frequent awakenings during the night. This can lead to a reduction in the total amount of REM sleep, which is essential for cognitive function, memory consolidation, and emotional regulation.
Treatment Options for Sleep Apnea: Treatment options for sleep apnea include continuous positive airway pressure (CPAP) therapy, oral appliances, and surgery in severe cases. CPAP therapy involves wearing a mask that delivers air pressure to keep the airway open during sleep. Oral appliances can help reposition the jaw or tongue to prevent airway obstruction. Surgery may be recommended in severe cases where other treatments have failed.
Restless Leg Syndrome
Restless Leg Syndrome, also known as RLS or Willis-Ekbom disease, is a disorder that affects the nervous system and causes an irresistible urge to move the legs. People with RLS often describe the sensation as a creeping, crawling or itching feeling in their legs. This feeling is usually worse at night or in the evening when trying to relax, which can make it difficult to fall asleep or stay asleep.
The exact cause of RLS is unknown, but it is thought to be related to an imbalance of the neurotransmitter dopamine in the brain. RLS can be present on its own (primary RLS) or as a secondary symptom of an underlying condition such as iron deficiency anemia, sleep apnea or pregnancy.
There are several treatment options available for RLS, including medications that increase dopamine levels in the brain, iron supplements for those with iron deficiency anemia, and lifestyle changes such as regular exercise and avoiding caffeine and alcohol. It is important to note that some medications used to treat RLS can actually worsen symptoms, so it is important to work closely with a healthcare provider to find the best treatment plan.
Unfortunately, RLS can significantly disrupt REM sleep. Due to the urge to constantly move the legs, people with RLS may have trouble relaxing and settling into sleep. This can lead to reduced total sleep time and reduced REM sleep time. Additionally, research has shown that people with RLS who experience a delay in falling asleep may have an increased risk of developing depression and anxiety. It is important to speak with a healthcare provider if you suspect you may have RLS to ensure proper diagnosis and treatment to improve sleep and overall quality of life.
Narcolepsy
Narcolepsy is a neurological sleep disorder characterized by excessive daytime sleepiness and a tendency to fall asleep suddenly and uncontrollably. It is caused by the brain’s inability to regulate sleep-wake cycles properly. People with narcolepsy often feel as though they haven’t slept at all, even after a full night’s rest.
Symptoms of Narcolepsy include:
– Sleep attacks that can occur at any time, even during inappropriate situations like driving or working
– Cataplexy, a sudden loss of muscle tone triggered by strong emotions like laughter, surprise or anger
– Sleep paralysis, the inability to move or speak during the transition between sleep and wakefulness
– Hypnagogic hallucinations, vivid and often terrifying dream-like experiences that occur during the onset of sleep
Narcolepsy often goes undiagnosed for years, as its symptoms are similar to those of other sleep disorders. People with the disorder may feel embarrassed or ashamed of their uncontrollable sleepiness, leading them to avoid seeking help.
There is no cure for narcolepsy, but there are medications that can help manage its symptoms. Stimulants, like amphetamines and modafinil, can help improve alertness and reduce sleep attacks. Antidepressants, specifically selective serotonin reuptake inhibitors (SSRIs), can help manage cataplexy and the other symptoms of the disorder.
Living with narcolepsy can be challenging, but making lifestyle adjustments like scheduling short naps in a quiet and safe environment and avoiding high-risk activities like driving can help manage its symptoms. Additionally, people with narcolepsy can benefit from support groups and counseling to help them cope with the emotional effects of the disorder.
Impact of Sleep Disorders on REM Sleep
Sleep disorders can have a significant impact on REM sleep, which is an important stage of sleep for a number of reasons. REM sleep is characterized by rapid eye movements and is typically associated with dreaming. During this stage of sleep, the brain is most active and the body becomes paralyzed to prevent acting out dreams. However, various sleep disorders can disrupt normal REM sleep patterns leading to negative impacts on sleep quality, overall health and well-being.
Disruption of Sleep Architecture
One of the main ways sleep disorders affect REM sleep is by disrupting the normal pattern of sleep stages. Sleep is divided into non-REM (NREM) and REM sleep stages, with regular cycling between them throughout the night. However, certain conditions, such as sleep apnea, can cause repeated interruptions to the sleep cycle leading to a reduction in the amount of deep NREM and REM sleep stages achieved each night. This reduced amount of REM sleep can affect the overall sleep quality and cause a feeling of excessive daytime sleepiness, cognitive impairment, irritability and other symptoms.
Reduced REM Sleep Time
Sleep disorders can also cause a reduction in REM sleep time, particularly in disorders such as insomnia, where individuals have difficulty falling and/or staying asleep. Insomniacs may experience shorter periods of time spent in REM sleep, leading to memory problems, mood disturbances, and a decreased ability to cope with stress. Similarly, in narcolepsy, REM sleep may occur soon after falling asleep, leading to individuals feeling groggy when they wake up in the morning.
Impaired Dreaming
REM sleep is also crucial for dreaming, which plays an important role in our mental health and processing of emotions. Sleep disorders such as restless leg syndrome, which involves the periodic movement of legs can interfere with REM sleep and causing discomfort that wakes an individual up from sleep leading to negative impacts on their mood and overall sleep quality.
It is important to recognize and understand the impact of sleep disorders on REM sleep. While disruptions to REM sleep may seem like a minor issue, it can disturb the overall architecture of sleep and lead to numerous negative health effects over time. It is essential to seek professional medical help to address sleep disorders and find effective treatment options to improve REM sleep quality and overall well-being.
Disruption of Sleep Architecture
When it comes to sleep disorders, one of the major ways they disrupt REM sleep is by causing a disruption in the overall sleep architecture. Sleep architecture refers to the natural progression of different stages of sleep during the night. During a normal, healthy night’s sleep, the body will cycle through the different stages of sleep multiple times. However, when something disrupts this natural progression, it can affect REM sleep in particular.
For example, insomnia, which is a common sleep disorder, can disrupt the natural progression of sleep by causing individuals to have difficulty falling asleep or staying asleep. This means that the body may not progress through the natural stages of sleep as it should, potentially leading to a decrease in REM sleep.
Similarly, sleep apnea, which is characterized by pauses in breathing during sleep, can also disrupt sleep architecture. This is because when an individual experiencing sleep apnea pauses their breathing, the body can be jolted out of deep sleep and forced to start the cycle over again. This can potentially decrease the amount of REM sleep an individual gets.
Restless leg syndrome and narcolepsy can also disrupt sleep architecture and affect REM sleep. Restless leg syndrome causes an uncontrollable urge to move the legs, which can lead to frequent waking during the night. Narcolepsy, on the other hand, can cause individuals to fall asleep suddenly and unexpectedly, leading to disrupted sleep cycles.
Any sleep disorder that disrupts the natural progression of sleep can potentially have a negative impact on REM sleep. This is because REM sleep typically occurs later in the night during longer periods of sleep. So, if sleep is disrupted, there may be less opportunity for an individual to enter REM sleep, leading to potential negative impacts on their health and well-being.
Reduced REM Sleep Time
During the stage of Rapid Eye Movement (REM) sleep, the brain is highly active and the body is essentially paralyzed. This stage of sleep is important for a number of reasons, including consolidating memory and regulating mood. However, many sleep disorders can disrupt REM sleep and reduce the amount of time spent in this stage of sleep.
One of the main culprits of reduced REM sleep time is insomnia. For individuals with insomnia, it can be difficult to fall asleep and stay asleep throughout the night. As a result, they may spend more time in lighter stages of sleep and less time in the important stages of deep and REM sleep. This can lead to an overall reduction in the amount of time spent in REM sleep.
Sleep apnea, which is characterized by pauses in breathing during sleep, can also lead to a reduction in REM sleep. When the body is struggling to breathe, it may wake up briefly and disrupt the natural sleep cycle. This can result in a reduction of overall REM sleep time.
Restless Leg Syndrome (RLS) is a neurological condition that causes an uncomfortable sensation in the legs and an irresistible urge to move them. RLS can lead to decreased REM sleep time because the sensations can make it difficult to fall asleep, and frequent movements can disrupt the natural sleep cycle.
Narcolepsy, a neurological disorder that causes sudden bouts of extreme sleepiness during the day, can also lead to a reduction in REM sleep. Individuals with narcolepsy may experience REM sleep abnormalities, such as entering REM sleep very quickly after falling asleep or experiencing a phenomenon known as “REM sleep intrusion,” where they enter REM sleep during the day when they are awake. This can result in a reduction in overall REM sleep time at night.
Reduced REM sleep time can have negative effects on both physical and mental health. It can lead to daytime fatigue, difficulty concentrating, and mood disturbances. It is important to identify and treat sleep disorders that disrupt REM sleep to ensure a healthy and restful night’s sleep.
Impaired Dreaming
During REM sleep, the brain is highly active and engaged in several important functions, including the consolidation of memories, emotional processing, and dreaming. However, sleep disorders can interfere with these crucial aspects of REM sleep, leading to impaired dreaming.
Insomnia can cause individuals to have difficulty falling asleep or staying asleep, which can ultimately lead to a reduction in the amount of time spent in REM sleep. This can result in fewer opportunities for dreaming to occur during the night, which can lead to a feeling of disconnection from one’s thoughts and emotions.
Sleep apnea can also negatively impact dreaming during REM sleep. Individuals with sleep apnea may experience frequent awakenings during the night due to pauses in breathing caused by obstructed airways. These interruptions can lead to a reduction in the total amount of time spent in REM sleep, resulting in fewer and shorter dream periods.
Restless leg syndrome is a disorder characterized by an uncontrollable urge to move one’s legs, often accompanied by unpleasant sensations in the limbs. These symptoms can become particularly problematic at night when individuals are trying to sleep, leading to disrupted sleep and a decrease in REM sleep time. As a result, individuals with restless leg syndrome may experience a reduction in vividness and frequency of dreaming.
Narcolepsy can also impact dreaming during REM sleep. Individuals with narcolepsy experience sudden and uncontrollable sleep attacks throughout the day, which can disrupt normal sleep patterns and lead to a shortage of REM sleep time at night. As a result, individuals with narcolepsy may experience fragmented dreaming, with dreams that are less vivid and more difficult to remember.
Impaired dreaming can be a significant consequence of sleep disorders. Disruptions to normal sleep patterns and a reduced amount of REM sleep can lead to a decrease in the frequency and intensity of dreams, which can negatively impact emotional processing and the consolidation of memories during sleep.
Treatment Options
When it comes to treating sleep disorders that disrupt REM sleep, there are a variety of options available. Here are some of the most common treatments:
Cognitive Behavioral Therapy for Insomnia: For those with insomnia, cognitive behavioral therapy (CBT) can be an effective treatment option. This type of therapy focuses on developing healthy sleep habits and addressing the underlying causes of insomnia, such as stress or anxiety. CBT may involve relaxation techniques, sleep restriction, and stimulus control.
Continuous Positive Airway Pressure Therapy for Sleep Apnea: Sleep apnea is often treated with continuous positive airway pressure (CPAP) therapy. This involves wearing a machine that delivers air pressure throughout the night, keeping the airway open and reducing the number of apnea events. CPAP therapy can greatly improve both the quantity and quality of sleep for those with sleep apnea.
Medications for Restless Leg Syndrome: Medications such as dopamine agonists, anticonvulsants, and iron supplements can be prescribed to relieve the symptoms of restless leg syndrome. These medications work by reducing the urge to move the legs and improving sleep quality.
Stimulants and Antidepressants for Narcolepsy: Narcolepsy, which causes excessive daytime sleepiness and sudden bouts of sleep, can be treated with stimulants such as modafinil or armodafinil. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) may also be prescribed to improve daytime alertness and reduce cataplexy (sudden loss of muscle tone).
It’s important to note that treatment options may vary depending on the individual and their specific sleep disorder. It’s best to consult with a healthcare professional to determine the most effective treatment plan.
Cognitive Behavioral Therapy for Insomnia
Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, or waking up too early. It affects millions of people worldwide and can have a significant impact on daily functioning and overall quality of life. While medication can be effective in treating insomnia, it often comes with side effects and the risk of addiction. Cognitive Behavioral Therapy (CBT), on the other hand, is a non-pharmacological approach that has been shown to be effective in improving sleep quality and helping to manage insomnia.
CBT for insomnia is a structured program that helps individuals identify and change negative thoughts and behaviors that may be contributing to sleep difficulties. It is typically delivered over several weeks and involves education about sleep hygiene, relaxation techniques, and stress management strategies.
One of the key components of CBT for insomnia is sleep restriction therapy. This involves limiting the amount of time spent in bed to match the amount of time spent sleeping. This can be challenging at first as it may result in feeling more tired during the day, but over time it can help to reset the body’s natural sleep-wake cycle and improve sleep efficiency.
Another component of CBT for insomnia is stimulus control therapy, which aims to strengthen the association between being in bed and sleeping. This involves creating a sleep-conducive environment, such as maintaining a consistent sleep schedule, avoiding stimulating activities before bedtime, and using the bed only for sleeping (rather than watching TV or working on a laptop).
CBT for insomnia has been shown to be effective in improving sleep quality, reducing the time it takes to fall asleep, and increasing total sleep time. It is also a relatively low-risk treatment option compared to medication. However, it may not be suitable for everyone, particularly those with underlying medical or psychological conditions that may be contributing to sleep difficulties. It is always recommended to consult with a healthcare professional to determine the best treatment approach for individual needs.
Continuous Positive Airway Pressure Therapy for Sleep Apnea
One of the most effective treatments for sleep apnea is Continuous Positive Airway Pressure (CPAP) Therapy. This treatment involves wearing a mask over the nose and/or mouth during sleep, which is connected to a machine that delivers a continuous stream of pressurized air. The air pressure keeps the airway open, preventing it from collapsing and causing breathing interruptions.
Studies have shown that CPAP therapy can improve the quality of sleep in individuals with sleep apnea, as well as reduce the frequency and severity of associated symptoms such as snoring, fatigue, and morning headaches. It can also lead to improvements in overall health and wellbeing, and reduce the risk of complications such as high blood pressure, stroke, and heart disease.
CPAP therapy is typically prescribed by a healthcare provider who specializes in sleep medicine. The provider will choose the appropriate mask and machine settings based on the individual’s needs, and the individual will be instructed on proper use and maintenance of the equipment.
While CPAP therapy can be highly effective, it may take some time for individuals to adjust to wearing the mask and sleeping with the machine. Some individuals may experience nasal congestion or dry mouth, but these symptoms can often be managed with adjustments to the settings or use of additional equipment.
In addition to CPAP therapy, there are other treatments available for sleep apnea such as positional therapy, oral appliances, and surgery. However, CPAP therapy remains the gold standard for treatment, particularly for individuals with moderate to severe sleep apnea.
Medications for Restless Leg Syndrome
Restless Leg Syndrome, or RLS, is a disorder characterized by an overwhelming urge to move one’s legs, especially when sitting or lying down. This can often disrupt sleep, including REM sleep. The exact cause of RLS is unknown, but medications can be effective in relieving symptoms.
Dopamine agonists are often prescribed for RLS. These drugs stimulate dopamine receptors in the brain, which can help reduce the urge to move one’s legs. Examples of dopamine agonists used for RLS include ropinirole, pramipexole, and rotigotine. It is important to note that these medications should be used only under the guidance of a medical professional, as they can have side effects such as dizziness, nausea, and even impulse control disorders.
Anticonvulsants are another class of drugs sometimes used to treat RLS. Gabapentin and pregabalin are two examples of anticonvulsants that can be effective for RLS. These medications work by reducing overactivity in the nervous system, which can help reduce the urge to move one’s legs. Side effects of anticonvulsants can include dizziness, drowsiness, and nausea.
Opioids may also be prescribed for RLS in some cases. These medications can help reduce the urge to move one’s legs by increasing levels of dopamine in the brain. Examples of opioids used for RLS include codeine and oxycodone. However, opioids can be habit-forming and have other serious risks associated with their use, so they are generally only used when other treatments have failed.
Medication can be an effective treatment option for RLS and can help improve the quality of REM sleep for those with the disorder. However, it is important to work closely with a medical professional to determine the most appropriate course of treatment and monitor for potential side effects.
Stimulants and Antidepressants for Narcolepsy
Narcolepsy is a sleep disorder characterized by excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), sleep paralysis, and hallucinations. Stimulants and antidepressants are the main medications used to treat narcolepsy.
Stimulants that are commonly used to treat narcolepsy include modafinil and methylphenidate. These medications work by increasing the levels of dopamine and norepinephrine in the brain, which helps to reduce excessive daytime sleepiness and improve alertness.
However, stimulants can have side effects such as increased heart rate, high blood pressure, and anxiety. It is important to discuss the risks and benefits of these medications with a healthcare professional.
Antidepressants that are used to treat narcolepsy include selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). These medications help to regulate the levels of neurotransmitters in the brain that are involved in sleep and mood.
Antidepressants can take several weeks to start working and may cause side effects such as nausea, dizziness, and sexual dysfunction. Like with stimulants, it is important to discuss the potential benefits and risks of these medications with a healthcare professional.
In addition to medication, lifestyle modifications such as regular sleep schedules, avoiding caffeine and alcohol, and regular exercise can also help to manage the symptoms of narcolepsy. It is important to work with a healthcare professional to develop a comprehensive treatment plan that meets the individual needs of each person with narcolepsy.
Conclusion
In conclusion, it is evident that sleep disorders play a significant role in disrupting REM sleep, which is a crucial stage in the sleep cycle. The consequences of such disruptions can have a profound impact on an individual’s physical and mental health, including their mood and ability to concentrate.
Common sleep disorders like insomnia, sleep apnea, restless leg syndrome, and narcolepsy can have a significant impact on REM sleep. These disorders can lead to a reduction in REM sleep time, disturbed sleep architecture, and impaired dreaming. As a result, individuals may experience fatigue, irritability, and difficulty with memory and concentration.
Fortunately, there are several treatment options available for sleep disorders such as cognitive-behavioral therapy for insomnia, continuous positive airway pressure therapy for sleep apnea, medications for restless leg syndrome, and stimulants and antidepressants for narcolepsy. Seeking professional help and diagnosis is the first step towards effective treatment and better sleep quality.
In all, it is important to take care of one’s sleep and recognize the potential consequences of sleep disorders, particularly their impact on REM sleep. Through proper diagnosis and treatment, individuals can improve their sleep quality, overall health, and well-being.
Frequently Asked Questions
What is the difference between REM sleep and non-REM sleep?
REM sleep is characterized by rapid eye movement, muscle paralysis, and vivid dreaming. Non-REM sleep has four stages and is marked by a decrease in brain activity and muscle tension.
Can sleep disorders affect both REM and non-REM sleep?
Yes, sleep disorders can affect both REM and non-REM sleep. However, different sleep disorders can have varying effects on these stages of sleep.
What are the symptoms of insomnia?
The symptoms of insomnia include difficulty falling or staying asleep, waking up too early in the morning, feeling tired upon waking, and daytime fatigue or sleepiness.
How does sleep apnea affect REM sleep?
Sleep apnea can cause interruptions in breathing during sleep, which can lead to a decrease in the amount of REM sleep a person gets. This can result in daytime sleepiness, fatigue, and difficulty concentrating.
What is restless leg syndrome?
Restless leg syndrome is a sleep disorder that causes uncomfortable sensations in the legs and an irresistible urge to move them. These symptoms can lead to difficulty falling and staying asleep.
Can narcolepsy affect REM sleep?
Yes, narcolepsy can affect REM sleep. People with narcolepsy experience excessive daytime sleepiness and can enter into REM sleep quickly, often without going through the stages of non-REM sleep first.
What are the effects of reduced REM sleep time?
Reduced REM sleep time can result in daytime sleepiness, fatigue, difficulty concentrating, and impaired memory function.
What is cognitive behavioral therapy?
Cognitive behavioral therapy is a type of talk therapy that focuses on identifying and changing negative thought patterns and behaviors that contribute to sleep disorders and other mental health issues.
How does continuous positive airway pressure therapy work?
Continuous positive airway pressure therapy delivers a steady stream of air pressure through a mask worn over the nose or mouth. This helps to keep the airway open and can reduce snoring and interruptions in breathing during sleep.
What are the side effects of medication for restless leg syndrome?
Common side effects of medication for restless leg syndrome can include nausea, dizziness, and fatigue. In rare cases, these medications can cause an increase in the risk of developing compulsive behaviors such as gambling or eating.