Many of us have experienced the unsettling feeling of being unable to move when we wake up from a deep sleep. It’s as if our body is in a state of paralysis, while our mind is fully awake and alert. This phenomenon is known as sleep paralysis, and it can be a frightening and confusing experience. Many people have searched for answers to what causes this strange condition, and scientists have been studying it for years. In this article, we will dive into the science of sleep paralysis during REM sleep, explore its causes and symptoms, and discuss various treatment options and prevention techniques. So, let’s explore the mysterious world of sleep paralysis together.
What is Sleep Paralysis?

Sleep paralysis is a perplexing and sometimes terrifying phenomenon that occurs when a person is unable to move or speak while falling asleep or waking up. It’s often accompanied by vivid hallucinations and a feeling of being held down or suffocated. This experience can be extremely distressing, leaving many to wonder what exactly sleep paralysis is and what causes it to happen. Let’s delve deeper into this fascinating and mysterious topic.
Definition of Sleep Paralysis
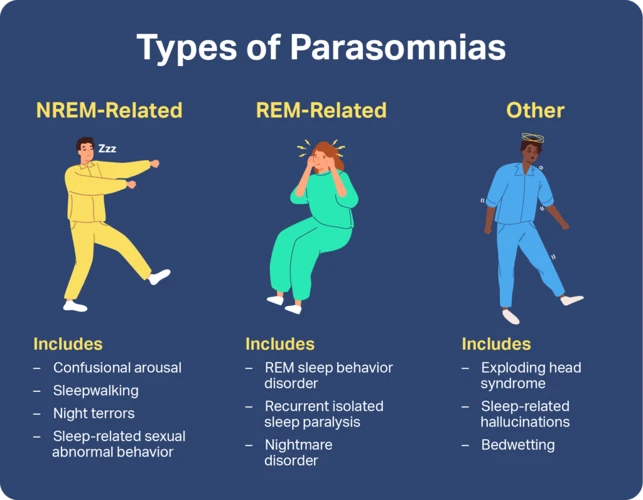
Sleep paralysis is a condition that affects the ability to move or speak during sleep. It is a type of parasomnia, which is a type of sleep disorder. During sleep paralysis, the body is unable to move, even when the mind is fully awake. This phenomenon can be very unsettling and can lead to feelings of fear and panic.
Some key characteristics of sleep paralysis include:
- Complete or partial paralysis of the body during sleep
- Feeling fully or partially awake during the episode
- Inability to move or speak during the episode
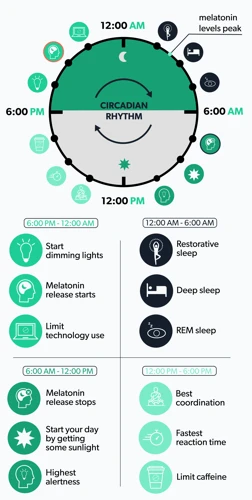
Sleep paralysis can occur at any time during the sleep cycle, but it typically occurs during REM sleep. REM (Rapid Eye Movement) sleep is a phase of the sleep cycle where the brain is very active, and the body is completely relaxed. This is the time when most dreams occur. During REM sleep, the body is essentially “turned off” to prevent you from acting out your dreams.
It’s important to note that sleep paralysis is not dangerous, and it is not associated with serious health conditions. However, it can be very distressing and may interfere with your sleep and daily functioning.
Sleep paralysis is a relatively common condition, and it can affect anyone. It is estimated that up to 8% of the general population experiences sleep paralysis at some point in their lives. The condition can occur on its own or as a symptom of another sleep disorder, such as narcolepsy.
If you experience sleep paralysis, it’s important to remember that it is a treatable condition. There are a variety of treatment options available, including lifestyle changes, medication, and therapy. With the right treatment, most people are able to manage their symptoms effectively and improve their quality of life.
The Science Behind Sleep Paralysis
During REM sleep, most of the muscles in our body are completely paralyzed to prevent us from physically acting out our dreams. Sleep paralysis occurs when this paralysis continues upon waking up from REM sleep, leaving individuals temporarily unable to move or speak despite being conscious. While the exact science behind sleep paralysis is not fully understood, researchers have identified several possible explanations.
One theory suggests that sleep paralysis occurs due to a failure in the timing of when muscle paralysis ends and the sleeper regains consciousness, causing a brief period of discoordination between brain signals and physical responses. Another theory suggests that sleep paralysis is caused by the brain still being in a “dream-like” state even after waking, and individuals may continue to experience hallucinations or vivid dream-like images even though they are fully conscious.
Interestingly, sleep paralysis has also been associated with increased activity in the amygdala, a part of the brain linked to fear and emotional regulation. This could explain why many individuals who experience sleep paralysis report feeling a sense of fear or impending doom during episodes.
Despite its potential link to fear and anxiety, sleep paralysis is actually a relatively common experience, with up to 50% of people reported having experienced it at least once in their lifetime. While it can be a frightening experience, understanding the science behind sleep paralysis can help individuals feel more at ease knowing that it is a relatively harmless condition.
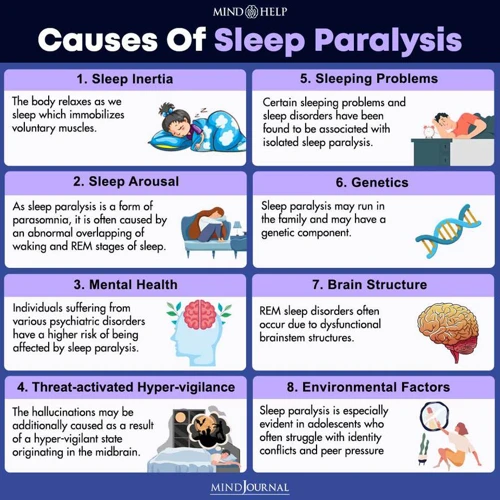
Causes of Sleep Paralysis
Understanding the underlying causes of sleep paralysis can be a perplexing journey into the intricate workings of the human brain and sleep cycles. It’s a phenomenon that leaves many people feeling puzzled and shaken, unsure of why their mind and body would react in such a way. But, by taking a closer look at the science behind sleep cycles and the factors that trigger sleep paralysis, we can gain a better understanding of this mysterious occurrence. Let’s explore the different elements that contribute to sleep paralysis and shed some light on what causes this perplexing phenomenon.
REM Sleep and Sleep Cycles
During REM (Rapid Eye Movement) sleep, the brain is highly active despite the body being in a state of muscle paralysis. This is the stage of sleep where most of our dreaming happens. A typical sleep cycle consists of five stages, including both REM and non-REM sleep. The stages of sleep are as follows:
| Stage | Description |
|---|---|
| Stage 1 | A light stage of sleep, where you can be easily awakened. Muscle activity slows and brain waves increase in frequency. |
| Stage 2 | Muscles relax further and brain waves become slower with occasional bursts of rapid waves. |
| Stage 3 | A deep stage of sleep, also known as slow-wave sleep (SWS). Breathing and heart rate slow down, and the body’s temperature drops. |
| Stage 4 | The deepest stage of sleep, also known as delta sleep. The body is in complete muscle paralysis. |
| REM Sleep | The stage of sleep where dreaming occurs and muscles are paralyzed. |
During the REM stage, the muscles of the body are essentially “turned off” to prevent individuals from acting out their dreams. This muscle paralysis is a natural process that occurs during sleep to keep the body still and prevent injury. However, this can also lead to the sensation of being unable to move or speak during sleep paralysis. Disorders such as sleep apnea, narcolepsy, and restless leg syndrome can interrupt sleep cycles and increase the likelihood of experiencing sleep paralysis during REM sleep. Understanding the various factors that can lead to sleep paralysis can help individuals obtain the appropriate care and treatment needed to prevent future episodes.
Other Factors that Trigger Sleep Paralysis
Several other factors can trigger sleep paralysis, including:
| Factor | Description |
|---|---|
| Narcolepsy | A sleep disorder that causes excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), and sometimes hallucinations. |
| Irregular sleep schedules | Shift work or jet lag can disrupt the body’s natural sleep pattern and increase the risk of sleep paralysis. |
| Stress and Anxiety | Mental stress and anxiety can trigger sleep paralysis, especially if the individual experiences panic attacks or has a history of trauma. |
| Substance abuse | Alcohol, nicotine, and certain medications can disrupt sleep and increase the likelihood of experiencing sleep paralysis. |
| Mental health conditions | Individuals with bipolar disorder, depression, or anxiety disorders are more likely to experience sleep paralysis. |
| Genetics | Some studies have suggested that certain genes may increase the risk of developing sleep paralysis. |
While these factors can increase the chance of experiencing sleep paralysis, it is important to note that not everyone who experiences them will develop this sleep disorder. If an individual has concerns about their risk for experiencing sleep paralysis, they should speak with a healthcare professional.
Symptoms of Sleep Paralysis
For those who have experienced it, sleep paralysis can be a deeply perplexing and unsettling phenomenon. The symptoms of sleep paralysis are often characterized by a sense of immobility, coupled with vivid hallucinations and a general feeling of terror or anxiety. These symptoms can be incredibly jarring, and can leave individuals feeling disoriented and confused. Despite the discomfort associated with sleep paralysis, however, it is important to remember that it is a relatively common occurrence, and one that can often be managed with the right treatment approach. In this section, we will explore the various symptoms associated with sleep paralysis, and discuss some strategies for diagnosis, treatment, and prevention.
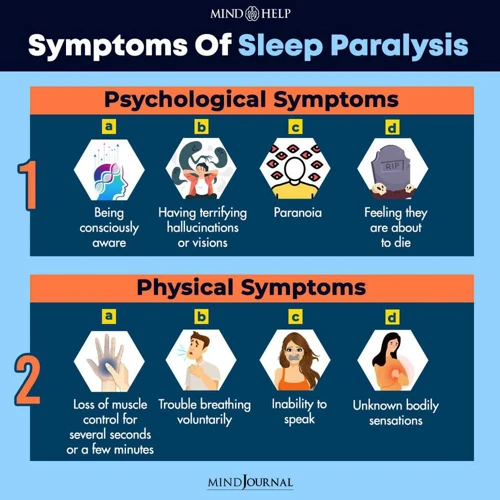
Physical Symptoms
During a sleep paralysis episode, a person may experience a variety of physical symptoms. These symptoms can differ from person to person, and can be influenced by a variety of factors including age, sleep position, and medical conditions. Some common physical symptoms of sleep paralysis include:
| Physical Symptoms | Description |
|---|---|
| Feeling of Pressure | Many people with sleep paralysis report feeling a sensation of pressure on their chest or body as if something is holding them down. This feeling can be accompanied by difficulty breathing or a sense of suffocation. |
| Muscle Weakness | During a sleep paralysis episode, the body is unable to move or function normally. This can cause a sense of muscle weakness or heaviness in the limbs. Some people may feel as if their muscles are paralyzed or frozen in place. |
| Visual Disturbances | Many people with sleep paralysis report seeing unusual or frightening visual disturbances during an episode. These can include hypnagogic or hypnopompic hallucinations, which are vivid and often terrifying images that may be accompanied by sounds or sensations. |
| Tactile Sensations | Some people with sleep paralysis may feel as if they are being touched or pulled by an unseen force. These tactile sensations can be accompanied by auditory hallucinations such as whispering or breathing sounds. |
| Difficulty Speaking or Swallowing | During an episode of sleep paralysis, the muscles of the mouth and throat may become relaxed, making it difficult to speak or swallow. Some people may experience choking sensations or feel as if they are unable to move their tongue or mouth. |
| Increased Heart Rate | During a sleep paralysis episode, the body may experience an increase in heart rate as a result of the stress and fear associated with the experience. This can further exacerbate feelings of panic or anxiety. |
The physical symptoms of sleep paralysis can be distressing and uncomfortable for those who experience them. It is important for individuals who suffer from sleep paralysis to seek medical attention and explore treatment options to prevent episodes and promote restful sleep.
Mental Symptoms
Sleep paralysis not only affects the body but also affects the mind, causing various **mental symptoms**. Here are some of the most common mental symptoms experienced during sleep paralysis:
- Fear: Many people experience intense fear during sleep paralysis, especially when combined with hallucinations.
- Anxiety: The fear and uncertainty caused by sleep paralysis can trigger anxiety and panic attacks in some individuals.
- Helplessness: Being unable to move or speak can cause feelings of helplessness and vulnerability.
- Disorientation: The experience of sleep paralysis and hallucinations can cause disorientation and confusion, making it difficult to distinguish between reality and the dream world.
- Depression: Recurring episodes of sleep paralysis can lead to depression, particularly if the individual experiences ongoing anxiety or fear of going to sleep.
It’s important to remember that while these mental symptoms can be distressing, they are a normal response to an abnormal situation. It is also worth noting that not all individuals will experience these symptoms, as everyone’s experience with sleep paralysis is different. In the next section, we will discuss how sleep paralysis can lead to hallucinations and nightmares.
Hallucinations and Nightmares
During sleep paralysis, it’s common to experience hallucinations and nightmares. These can be extremely distressing and can affect a person’s quality of life. Here are some common hallucinations and nightmares during sleep paralysis:
- Visual hallucinations: You may see people, animals or objects that aren’t actually there. These hallucinations can feel extremely vivid and real, and can be scary, especially if the hallucination is threatening in nature.
- Tactile hallucinations: You may feel as if someone is touching you, holding you down or even choking you. These hallucinations can be extremely distressful and can make it feel like you aren’t in control of your body.
- Auditory hallucinations: You may hear sounds like footsteps or whispers, which can add to the feeling of being watched or attacked.
- Nightmares: During sleep paralysis, you may experience vivid and often terrifying nightmares. It’s not uncommon for these nightmares to feel extremely vivid, and even after waking up, it can be hard to shake the feeling that they were real.
These hallucinations and nightmares can have a significant impact on a person’s mental well-being. It’s not uncommon for people who experience sleep paralysis to feel anxious or depressed, and to develop a fear of going to sleep. It’s important to speak to a healthcare professional if you are experiencing these symptoms so that they can provide you with appropriate treatment and support.
Diagnosing Sleep Paralysis
As sleep paralysis can be a frightening and confusing experience, it’s important to seek a medical diagnosis in order to rule out any underlying medical or mental health conditions. A diagnosis can also provide insight into the frequency and severity of sleep paralysis episodes, as well as potential treatment options. Let’s explore some of the methods healthcare professionals use to diagnose sleep paralysis.
Sleep Studies
Sleep studies are a type of diagnostic test that are often used to diagnose sleep disorders, including sleep paralysis. These tests are typically done in a sleep laboratory, where a person is monitored overnight while they sleep. There are several different types of sleep studies that can be used to diagnose sleep paralysis and other sleep-related disorders, including:
- Polysomnography (PSG): This test involves monitoring a person’s brain waves, eye movements, muscle activity, heart rate, and breathing during sleep. It can help doctors determine if a person is experiencing sleep paralysis, as well as the severity of the condition.
- Multiple Sleep Latency Test (MSLT): This test involves monitoring a person’s ability to fall asleep during the day. It can help doctors determine if a person is experiencing excessive daytime sleepiness, which can be a symptom of sleep paralysis.
- Actigraphy: This test involves wearing a small device on the wrist that measures movement and provides information about a person’s sleep patterns.
- Home Sleep Testing: This test involves using a portable device to monitor a person’s breathing, oxygen levels, and heart rate while they sleep at home. It is typically used to diagnose sleep apnea, but can also be used to diagnose sleep paralysis in some cases.
By performing these tests, doctors can obtain valuable information about a person’s sleep patterns and help determine the underlying causes of sleep paralysis. This information can then be used to develop a personalized treatment plan that is tailored to the individual’s needs.
Medical Tests
Medical Tests play an important role in diagnosing Sleep Paralysis. There are various tests that healthcare providers may recommend in order to rule out any other underlying medical condition that might be present along with Sleep Paralysis. Here are some of the medical tests that might be performed:
| Tests | Purpose |
|---|---|
| Polysomnography | Polysomnography is a type of sleep study that is conducted overnight with the help of sensors placed on the body, including the scalp, face, chest, limbs, and fingers. It helps to evaluate various aspects of sleep, such as body position, eye movements, brain activity, and muscle tone. |
| Magnetic Resonance Imaging (MRI) | MRI is a type of imaging test that uses strong magnetic fields and radio waves to produce detailed pictures of the body. It helps to detect any structural abnormalities in the brain or the spinal cord, which might be the reason behind the occurrence of Sleep Paralysis. |
| Electroencephalography (EEG) | EEG is a non-invasive test that measures the electrical activity of the brain using small, flat metal discs called electrodes that are attached to the scalp. It helps to detect any abnormalities in brain waves that might be related to Sleep Paralysis. |
| Multiple Sleep Latency Test (MSLT) | MSLT is a type of sleep study that evaluates the tendency of a person to fall asleep during the day. It involves taking short naps at different intervals during the day, and it helps to detect any abnormal sleepiness that might be related to Sleep Paralysis. |
It is important to note that medical tests alone cannot diagnose Sleep Paralysis. A combination of physical and mental evaluations, along with a detailed medical history, is necessary to diagnose Sleep Paralysis accurately. Once the healthcare provider has diagnosed Sleep Paralysis, a suitable treatment plan can be outlined for the patient.
Mental Health Evaluations
Mental health evaluations are sometimes conducted when a person experiences sleep paralysis. These evaluations are important to identify any underlying mental health conditions that may contribute to the development of sleep paralysis.
During a mental health evaluation, a mental health professional will assess the person’s mental and emotional well-being. They may use various techniques, including interviews and surveys, to gather information about the person’s symptoms, medical history, and family history.
The information gathered during a mental health evaluation can be used to:
| Assess for underlying mental health conditions | Mental health professionals will assess for underlying conditions such as anxiety disorders and depression, which can contribute to the development of sleep paralysis. |
|---|---|
| Develop a treatment plan | Based on the results of the evaluation, a mental health professional can develop a treatment plan that addresses the underlying mental health condition contributing to the person’s sleep paralysis. |
| Rule out other conditions | Sleep paralysis can sometimes be a symptom of other underlying conditions such as narcolepsy, and a mental health evaluation can help rule out these possibilities. |
| Provide support and guidance | Mental health professionals can provide support and guidance to the person experiencing sleep paralysis, and offer coping strategies to help manage and reduce the frequency of episodes. |
It is important to note that mental health evaluations are just one component in the diagnosis and treatment of sleep paralysis, and that a comprehensive medical evaluation is also necessary to identify any potential physical causes.
Treatment Options for Sleep Paralysis
For those who experience sleep paralysis, it can be a truly terrifying and unsettling experience. Fortunately, there are treatment options available that can help alleviate the symptoms and improve overall sleep quality. These treatments range from lifestyle changes to medications to therapy, and can be tailored to each individual’s unique needs. In this section of the article, we will explore the different treatment options for sleep paralysis and discuss the potential benefits and drawbacks of each.
Lifestyle Changes
Making certain lifestyle changes can also help prevent and manage sleep paralysis. Here are some recommendations:
- Improving sleep habits: It is important to maintain a regular sleep schedule and create a relaxing bedtime routine in order to promote healthy sleep habits. This involves avoiding caffeine and alcohol before bed, as well as avoiding eating heavy meals close to bedtime.
- Managing stress and anxiety: Since stress and anxiety can trigger sleep paralysis, it’s important to find ways to manage those feelings. Techniques like deep breathing, meditation, and yoga can be helpful in reducing stress levels.
- Creating a comfortable sleep environment: Setting up a comfortable sleep environment can help promote better sleep quality, which may reduce the risk of sleep paralysis. This can involve keeping the bedroom dark, cool, and quiet.
- Avoiding sleep on the back: Studies have shown that being in a supine position (lying on the back) during sleep can increase the risk of sleep paralysis. It’s recommended to avoid sleeping on the back and instead try sleeping on the side.
By implementing these lifestyle changes, individuals may be able to reduce the frequency and severity of sleep paralysis episodes. However, if sleep paralysis is interfering with daily life, it’s important to seek medical attention and discuss other treatment options with a healthcare professional.
Medications
When it comes to treating sleep paralysis, there are a few medications that can be prescribed by a doctor. It’s important to note that while medications can be effective, they should only be used under professional guidance as some can have side effects and may not be suitable for everyone.
1. Antidepressants: Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) can be prescribed to help regulate sleep and reduce the frequency of sleep paralysis episodes. These medications work by altering the balance of chemicals in the brain that affect mood and sleep.
2. Benzodiazepines: Benzodiazepines are a type of medication that work by calming the central nervous system. They can help alleviate anxiety and promote relaxation, which can be helpful for people who experience sleep paralysis as a result of stress or anxiety. However, they can be habit-forming, so they should only be used under professional guidance and for short periods of time.
3. Melatonin: Melatonin is a hormone that regulates the sleep-wake cycle. It can be used to help improve the quality of sleep and reduce the frequency of sleep paralysis episodes. However, it should only be used under professional guidance as it can interact with other medications and may not be suitable for everyone.
4. Stimulants: Stimulant medications such as modafinil and armodafinil can be used to reduce the frequency of sleep paralysis episodes. They work by promoting wakefulness and reducing the amount of time spent in REM sleep. However, they can have side effects such as headaches, anxiety, and insomnia and should only be used under professional guidance.
It’s important to note that medication should not be the sole form of treatment for sleep paralysis. A combination of medication and therapy, as well as lifestyle changes, can be more effective in managing the condition. It’s also important to discuss any concerns or questions about medications with a healthcare professional.
Therapy
People who experience sleep paralysis may find relief through various forms of therapy. Here are some examples:
- Cognitive Behavioral Therapy (CBT): This form of therapy involves identifying and changing negative thought patterns and behaviors that could be contributing to sleep paralysis. A therapist may work with an individual to develop coping mechanisms or relaxation techniques to reduce the impact of sleep paralysis episodes.
- Sleep Hygiene Education: A healthcare provider may recommend learning about and implementing certain healthy sleep habits, such as sticking to a regular sleep schedule, avoiding caffeine and alcohol before bedtime, and ensuring that the sleep environment is cool, dark, and quiet.
- Lucid Dreaming Therapy: Some people who experience sleep paralysis also have an interest in lucid dreaming, which involves being aware that you are dreaming and having some control over the dream. A therapist may work with an individual to develop techniques for inducing and controlling lucid dreams, which can help reduce the fear and anxiety associated with sleep paralysis.
- Hypnotherapy: Hypnotherapy involves guided relaxation and focused attention to help an individual enter a trance-like state. A therapist may use this technique to help an individual identify and address any underlying emotional or psychological factors that may be contributing to sleep paralysis.
It’s important to note that therapy can be an effective tool for managing sleep paralysis, but it may not completely eliminate episodes. Consulting with a healthcare provider or mental health professional can help an individual determine the best course of treatment for their specific situation.
Prevention and Management of Sleep Paralysis
As sleep paralysis can be a terrifying experience for many individuals, it is important to understand the various prevention and management techniques that can be implemented. By taking steps to improve sleep hygiene, manage stress and anxiety, and control the sleep environment, individuals may be able to reduce the frequency and severity of sleep paralysis episodes. In this section, we will explore some of the strategies that can be used to prevent and manage sleep paralysis.
Sleep Hygiene
One of the most effective ways to prevent and manage sleep paralysis is to maintain good sleep hygiene. This includes developing habits and practices that promote better quality sleep.
Some tips for good sleep hygiene are:
| Tip | Description |
|---|---|
| Stick to a consistent sleep schedule | Go to bed and wake up at the same time every day, even on weekends. |
| Create a comfortable sleep environment | Make sure the room is dark, cool, and quiet. Use comfortable bedding and a supportive mattress. |
| Avoid stimulating activities before bed | Avoid using electronic devices or watching TV at least one hour before bedtime. |
| Establish a relaxing bedtime routine | Take a warm bath, read a book, or listen to calming music before bed to help relax the mind. |
| Limit caffeine and alcohol intake | Avoid consuming caffeine or alcohol close to bedtime as they can disrupt sleep. |
| Exercise regularly | Regular exercise can improve sleep quality, but avoid intense exercise close to bedtime. |
| Manage stress and anxiety | Practice relaxation techniques, such as deep breathing or meditation, to reduce stress and anxiety before bed. |
Following these tips can help improve sleep quality and reduce the risk of experiencing sleep paralysis. It’s also important to consult with a healthcare professional if sleep paralysis persists or interferes with daily functioning.
Managing Stress and Anxiety
Living with sleep paralysis can be incredibly stressful and anxiety-provoking. Fortunately, there are various ways to manage stress and anxiety that can help reduce the frequency and intensity of sleep paralysis episodes.
1. Practice relaxation techniques: Relaxation techniques such as deep breathing, meditation, and progressive muscle relaxation can help reduce overall stress and anxiety levels. These techniques can be practiced before bed or during an episode of sleep paralysis to help calm the mind and body.
2. Exercise regularly: Exercise is a great way to reduce stress and anxiety levels. Regular exercise can help improve overall physical and mental health, which can in turn reduce the frequency and intensity of sleep paralysis episodes.
3. Seek support: Talking to a trusted friend, family member, or mental health professional can be incredibly helpful for managing stress and anxiety related to sleep paralysis. Support groups for people with sleep disorders may also be available in your area.
4. Identify triggers: Keep a journal or record of when sleep paralysis episodes occur and any possible triggers, such as stress, certain foods or drinks, or lack of sleep. Identifying and avoiding these triggers can help reduce the frequency and intensity of sleep paralysis episodes.
5. Practice good sleep hygiene: Maintaining good sleep hygiene is important for reducing stress and anxiety related to sleep paralysis. This includes things like establishing a regular sleep schedule, avoiding caffeine and alcohol before bedtime, and creating a comfortable sleep environment.
By implementing these strategies, individuals with sleep paralysis can manage their stress and anxiety levels and reduce the frequency and severity of episodes.
Controlling Sleep Environment
One of the methods for preventing and managing sleep paralysis is by controlling the sleep environment. This involves ensuring that the bedroom is a comfortable and relaxing place for sleep. Here are some ways to achieve this:
| Technique | Explanation |
|---|---|
| Reduce noise | External noise can be a major factor that disrupts sleep. Try using earplugs, soundproof curtains, or a white noise machine to create a calmer environment. |
| Ensure darkness | Light can interfere with the body’s natural sleep cycle, so it’s important to create a dark environment. Consider using blackout curtains or an eye mask to block out any light from outside sources. |
| Use comfortable bedding | Comfortable bedding is critical to good sleep. Choose sheets and blankets made from breathable, comfortable materials such as cotton or bamboo, and invest in a mattress and pillows that provide adequate support for your body. |
| Adjust temperature | The ideal sleep environment is cool and comfortable. Adjust the temperature in the room to ensure it’s not too hot or too cold for sleep. Keep a fan or air conditioning unit on to create a gentle breeze and circulate the air in the room. |
| Clear clutter | A cluttered bedroom can make it difficult to relax and fall asleep. Try to keep the space as organized as possible, and remove any unnecessary items that may be causing stress or anxiety. |
By taking steps to create a peaceful and calm sleeping environment, individuals who experience sleep paralysis may be able to lessen the frequency and severity of episodes.
Conclusion
In conclusion, experiencing sleep paralysis can be a terrifying and unsettling experience for anyone. However, by understanding the causes, symptoms, and treatment options available, individuals can take steps to manage and prevent this phenomenon from occurring. It is important to remember that sleep paralysis is not indicative of a larger medical condition or mental health issue, but rather a normal process that occurs during REM sleep.
It is important to engage in good sleep hygiene practices such as maintaining a regular sleep schedule, creating a comfortable sleep environment and managing stress and anxiety. This can help to reduce the likelihood of sleep disturbances such as sleep paralysis. In some cases, medication or therapy may be recommended to manage symptoms of sleep paralysis.
It is also important for individuals to seek medical attention if they experience persistent sleep paralysis or if their symptoms are impacting their daily life. A doctor can perform a sleep study or other medical tests to ensure that sleep paralysis is not indicative of an underlying sleep disorder or other medical condition.
Overall, with the right knowledge and strategies, sleep paralysis can be managed and controlled. By taking care of our physical and mental health, we can reduce the likelihood and impact of sleep disturbances and enjoy restful, rejuvenating sleep.
Frequently Asked Questions
What is the difference between sleep paralysis and regular dreaming?
Sleep paralysis occurs during REM sleep and involves the inability to move while still aware of one’s surroundings. Dreaming, on the other hand, can occur during any stage of sleep and involves various sensory experiences and often movement.
Can anyone experience sleep paralysis?
Yes, anyone can experience sleep paralysis. However, it is more common in individuals who have a history of sleep disorders, mental health conditions, or a family history of sleep paralysis.
How long does a typical episode of sleep paralysis last?
A typical episode of sleep paralysis can last anywhere from a few seconds to several minutes.
Are hallucinations a common symptom of sleep paralysis?
Yes, hallucinations are a common symptom of sleep paralysis. They can range from mild visual distortions to frightening images and sounds.
Can sleep paralysis be dangerous?
While sleep paralysis itself is not dangerous, the accompanying feelings of fear and panic can be distressing. Additionally, some individuals may be at risk for injury if they experience sleep paralysis while driving or operating heavy machinery.
Can medication trigger sleep paralysis?
Yes, certain medications can trigger sleep paralysis. These include antidepressants, antihistamines, and medications used to treat Parkinson’s disease.
Is sleep paralysis contagious?
No, sleep paralysis is not contagious. It is a natural occurrence that happens during REM sleep.
Can sleep paralysis be cured?
While there is no cure for sleep paralysis, it can be managed through certain lifestyle changes, medications, and therapy.
Can sleep paralysis be a sign of a more serious underlying condition?
While sleep paralysis itself is not a sign of a serious underlying condition, it can be a symptom of narcolepsy, a neurological disorder that affects the sleep-wake cycle.
Is there a way to prevent sleep paralysis?
While there is no guaranteed way to prevent sleep paralysis, practicing good sleep hygiene, managing stress and anxiety, and controlling the sleep environment can help reduce the risk of experiencing an episode.