Nightmares are a common occurrence for many, but for those who have experienced trauma, they can be an all-consuming and unbearable aspect of life. The link between trauma and nightmares can be a perplexing and overwhelming experience, leaving many to ask why their minds are plagued with such vivid and disturbing images. In this article, we will explore the science behind nightmares, the connection between trauma and their frequency, and the different methods of managing trauma-related nightmares. By understanding the underlying mechanisms at work, we can begin to untangle the relationship between trauma and nightmares and find ways to alleviate their impact on our lives.
The Science Behind Nightmares
Have you ever woken up in the middle of the night, drenched in sweat, heart racing, after a really vivid and terrifying dream? Nightmares are a common occurrence, affecting up to 90% of adults at some point in their lives. They can leave us feeling shaken and anxious, but what causes them? The science behind nightmares is still being studied, but researchers have identified some key factors that may contribute to their occurrence. Understanding the science behind nightmares can help us better manage and cope with them.
Definition of Nightmares
When we go to sleep, we hope for a peaceful and restful night. However, for some individuals, this may not be the case. Nightmares can happen to anyone, and they are a natural and normal part of the sleep cycle. According to the International Classification of Sleep Disorders (ICSD), nightmares are characterized by vivid, frightening dreams that usually involve threats to survival, security, or self-esteem. Nightmares usually occur during the REM (Rapid Eye Movement) stage of sleep, which is the stage where the brain is most active, and most dreaming occurs.
It’s essential to note that not all bad dreams are nightmares, and they aren’t always caused by trauma. Sometimes, nightmares can be caused by other factors such as medications, alcohol or drug use, or even underlying medical conditions such as sleep apnea. However, when nightmares occur frequently and are associated with traumatic experiences, they can significantly impact an individual’s mental and physical well-being. Ongoing nightmares can lead to sleep deprivation, which can affect an individual’s mood, concentration, and memory.
To diagnose nightmares, a medical professional will need to evaluate the individual’s sleep history and frequency of nightmares. A sleep study may also be conducted to assess the individual’s sleep cycle and to rule out other potential causes. It’s crucial to seek medical attention if nightmares are affecting an individual’s ability to function during the day or causing significant distress.
Impact of Trauma on Sleep
The Impact of Trauma on Sleep
Trauma can have a significant impact on a person’s sleep, leading to an increased risk of nightmares and other sleep disturbances. Here are some ways in which trauma can impact sleep:
- Hyperarousal: Individuals who have experienced trauma may have an enhanced state of arousal that can persist long after the traumatic event. This can make it difficult to fall asleep and stay asleep, and it can cause a person to wake up frequently during the night.
- Anxiety: Trauma survivors may experience high levels of anxiety, which can make it difficult to relax and fall asleep. Anxiety can also cause a person to wake up during the night with feelings of fear or panic.
- Flashbacks: Trauma survivors may experience vivid and disturbing flashbacks of the traumatic event, which can occur during the day or night. Nighttime flashbacks can be especially distressing and can disrupt sleep.
- Nightmares: Trauma survivors may experience frequent nightmares that are directly related to the traumatic event. These nightmares can be extremely vivid and realistic, and they can cause a person to wake up feeling scared, anxious, or sad.
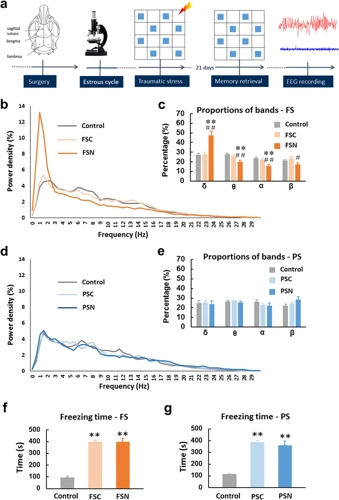
- Increased REM Sleep: Trauma can lead to an increase in rapid eye movement (REM) sleep, which is the stage of sleep that is most closely associated with dreaming. This can result in an increase in dream activity, including nightmares.
It is important to note that not all trauma survivors will experience sleep disturbances, and those who do may have different types and degrees of sleep problems. However, sleep disturbances are common among trauma survivors and can have a significant impact on their quality of life.
The Role of REM Sleep
During REM (Rapid Eye Movement) sleep, the brain becomes more active and consumes more oxygen than in non-REM stages. It is during this stage that most dreaming occurs, and it is also when the body is more relaxed and immobile. REM sleep is essential for emotional processing and memory consolidation, which means that it plays a critical role in our ability to process and overcome trauma.
During REM sleep, the brain processes emotional and traumatic experiences by forming connections between memories and emotions. This integration helps individuals to make sense of and cope with their experiences. Without proper REM sleep, traumatic memories can remain unprocessed and lead to further emotional distress.
Moreover, REM sleep also helps to regulate emotions and reduce their intensity. A lack of REM sleep can cause heightened emotional reactivity, which increases the risk of developing anxiety and mood disorders. It is crucial to have sufficient quality of REM sleep to maintain good emotional health.
Interestingly, researchers have found that disruptions in REM sleep can lead to an increase in nightmares. This suggests that nightmares and trauma-related dreams may be caused by the brain’s attempt to process and cope with traumatic experiences during REM sleep. It also highlights the importance of REM sleep in regulating emotions and preventing the development of PTSD.
In summary, REM sleep is critical for emotional processing, memory consolidation, and regulating emotions. Disruptions in REM sleep can have a significant impact on an individual’s psychological well-being, including an increase in nightmare frequency.
The Connection Between Trauma and Nightmares
For individuals who have experienced trauma, nightmares can be a frequent and distressing occurrence. The types of trauma that can lead to nightmares are varied, ranging from physical violence to emotional abuse. Despite the various forms of trauma, the connection between trauma and nightmares is a well-established phenomenon that has been extensively studied. The mechanisms that lead to nightmares following trauma are complex, involving both psychological and physiological factors. Understanding this connection is crucial for individuals who have experienced trauma and are struggling with nightmares as a result.
Types of Trauma
Experiencing trauma can greatly impact one’s mental and emotional well-being, and can even manifest as frequent nightmares. There are various types of trauma that individuals can experience, each with their own unique set of symptoms and effects.
One type of trauma is physical trauma, which can result from accidents, injuries, or violence. This type of trauma can cause nightmares related to the event or injury, and can also lead to chronic pain and disrupted sleep patterns.
Sexual trauma, such as sexual assault or abuse, can also increase the frequency of nightmares. This type of trauma can be particularly difficult to cope with and may require specialized treatment.
Emotional or psychological trauma can result from various experiences, such as the loss of a loved one or a traumatic event, and can lead to nightmares related to the experience or feelings of anxiety and depression.
Environmental trauma, such as natural disasters or exposure to environmental toxins, can also result in nightmares and disruptive sleep patterns.
It is important to note that everyone experiences trauma differently, and the type of trauma someone experiences can greatly impact their mental and emotional well-being. Seeking support and treatment can help individuals cope with the effects of trauma, including frequent nightmares.
Post Traumatic Stress Disorder
Post Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event. The condition is characterized by feelings of fear, anxiety and helplessness, and can last for months or even years after the event.
PTSD can be triggered by any event that causes an individual to feel intense fear, horror, or helplessness. This can include natural disasters, accidents, violence, or military combat. It is important to note that not everyone who experiences trauma will go on to develop PTSD, but it is a common outcome in those who do.
The symptoms of PTSD can be grouped into four categories: re-experiencing, avoidance, arousal and reactivity, and mood and cognition. Individuals with PTSD may experience flashbacks, nightmares, and intrusive thoughts related to the traumatic event. They may also avoid triggers that remind them of the event and have difficulty sleeping or concentrating. In severe cases, individuals with PTSD may experience panic attacks or become isolated and withdrawn.
PTSD can have a significant impact on an individual’s quality of life, causing difficulties in relationships, work, and daily activities. Thus, it is important to seek treatment if symptoms persist and are interfering with daily functioning. Treatment options for PTSD may include therapy, medication, or a combination of both. Cognitive behavioral therapy (CBT) is a common form of therapy used to treat PTSD, which involves changing negative thought patterns and behaviors related to the traumatic event. Medications such as antidepressants can also be used to alleviate symptoms of PTSD.
PTSD is a serious and complex mental health condition that can occur after experiencing or witnessing a traumatic event. If you or someone you know is experiencing symptoms of PTSD, seek professional help to manage and alleviate symptoms.
Psychological Mechanisms
When it comes to understanding the link between trauma and nightmares, it’s essential to explore the psychological mechanisms at play. Trauma is known to impact the way the brain processes and stores memories, leading to an overactivation of the amygdala, the part of the brain responsible for processing emotions like fear and anxiety. As a result, individuals who have experienced trauma may be more likely to experience nightmares where they relive the traumatic event.
Additionally, trauma can lead to a disruption in sleep architecture, specifically in the Rapid Eye Movement (REM) stage of sleep. During REM sleep, the brain is processing emotions and consolidating memories, which can also increase the likelihood of traumatic material resurfacing during nightmares.
Studies have also shown that individuals who experience trauma may have higher levels of hypervigilance and arousal, leading to increased stress and anxiety levels, which can exacerbate nightmare frequency. This heightened state of arousal can also lead to an increased sensitivity to environmental stimuli, making individuals more susceptible to experiencing nightmares.
Trauma can affect an individual’s sense of safety and security, leading to an increased risk of developing Post Traumatic Stress Disorder (PTSD). Individuals with PTSD may experience frequent nightmares related to their trauma, as well as other symptoms like anxiety and flashbacks.
Understanding the psychological mechanisms involved in the link between trauma and nightmares is crucial in developing effective treatment options for individuals who may be struggling with the aftermath of a traumatic event.
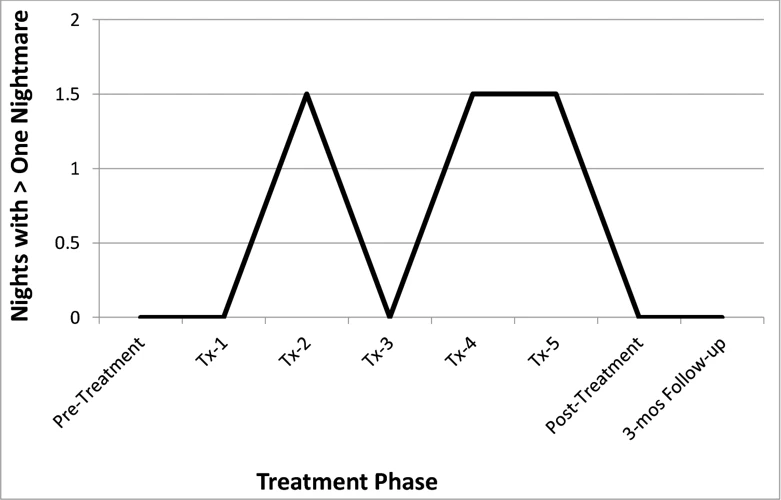
Managing Trauma-Related Nightmares
After understanding the link between trauma and nightmare frequency, it can be difficult to manage the persistent nightmares that may arise from past trauma. However, there are various treatment options, lifestyle changes, and coping strategies that can help individuals regain control over their sleep and reduce the frequency and intensity of their trauma-related nightmares. Let’s explore some ways to manage these nightmares and improve overall sleep quality.
Treatment Options
Treatment Options for Trauma-Related Nightmares are varied and can be tailored to the individual’s specific needs. Here are some of the most common options:
| Treatment Option | Description |
|---|---|
| Therapy: | One of the most effective treatments for trauma-related nightmares is therapy. Cognitive Behavioral Therapy (CBT) and Exposure Therapy are two common approaches. CBT helps individuals identify and challenge negative thought patterns related to their trauma, while Exposure Therapy gradually exposes them to the source of their fear until they develop new coping skills. |
| Medication: | Medication can be helpful for some individuals dealing with trauma-related nightmares. Antidepressants and anti-anxiety medications can reduce the frequency and intensity of nightmares. It is important to consult with a doctor before taking any new medication. |
| Hypnotherapy: | Hypnotherapy is a type of therapy that uses relaxation techniques to help individuals access their unconscious thoughts and memories. It has been used to treat trauma-related nightmares by helping individuals confront their fears and develop new coping mechanisms. |
| Eye Movement Desensitization and Reprocessing (EMDR): | EMDR is a type of therapy that helps individuals process traumatic memories by focusing on eye movements or other types of bilateral stimulation. It has been found to be effective in reducing the frequency and intensity of nightmares. |
It is important to note that finding the right treatment option may take time and may require a combination of approaches. It is always best to consult with a healthcare professional before beginning any treatment.
Lifestyle Changes
Making lifestyle changes can be an effective way to manage trauma-related nightmares. Consider incorporating the following changes into your daily routine:
- Establish a Consistent Sleep Schedule: Going to bed and waking up at the same time each day can help regulate your sleep cycle and improve the quality of your sleep. This may involve adjusting your schedule and sticking to it, even on weekends and holidays.
- Evaluate Your Sleeping Environment: Assess your sleeping environment and eliminate as many distractions as possible. This may include removing electronic devices from the bedroom or using noise-cancelling earplugs to block out background noise
- Reduce Stimulants: Limit caffeine and alcohol consumption, especially before bedtime. These substances can interfere with your sleep patterns and make it difficult to fall asleep or remain asleep throughout the night.
- Engage in Relaxation Techniques: Experiment with relaxation techniques such as deep breathing, meditation or yoga to help reduce stress and anxiety levels. Engaging in a calming activity before bedtime can also help promote a better quality of sleep.
- Create a Bedtime Ritual: Establishing a bedtime routine can help signal to your body that it is time to relax and fall asleep. This may include taking a warm bath or shower, reading a book, or practicing your favorite relaxation technique.
By incorporating these lifestyle changes, you may be able to manage your nightmares and enjoy a more peaceful night’s sleep. However, if your nightmares persist or are causing you significant distress, it’s important to speak with a healthcare provider to explore additional treatment options.
Coping Strategies
When dealing with trauma-related nightmares, there are several coping strategies that can be helpful. Coping strategies are techniques or behaviors that an individual can do to manage their symptoms, reduce their distress, and recover from the impact of the trauma. The following table highlights some potential coping strategies for nightmare sufferers:
| Coping Strategies | Description |
|---|---|
| Grounding Techniques | Grounding techniques are sensory-based strategies that can help individuals feel more connected to the present moment. Some examples include deep breathing, progressive muscle relaxation, and visualization exercises. |
| Sleep Hygiene | Improving sleep hygiene can lead to better quality sleep, which can reduce the frequency and intensity of nightmares. Suggestions for improving sleep hygiene include creating a calming bedtime routine, avoiding caffeine and electronics in the evening, and keeping the bedroom cool and dark. |
| Journaling | Writing down one’s thoughts and feelings about the trauma and related nightmares can be cathartic and help individuals process their experiences. Additionally, keeping a dream journal can help individuals identify triggers for their nightmares and themes that may require further exploration in therapy. |
| Mindfulness-Based Therapies | Mindfulness-based therapies, such as mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), can help individuals cultivate awareness and acceptance of their thoughts and feelings, which can lead to a reduction in anxiety and stress. These therapies may also improve sleep quality and reduce nightmare frequency. |
| Support Groups | Participating in a support group can provide individuals with a safe and validating environment where they can connect with others who have had similar experiences. Support groups can also offer practical advice and emotional support, as well as help reduce feelings of isolation and shame. |
It’s important to note that not all coping strategies will be effective for every individual. It may take some trial and error to find the strategies that work best for each person. Additionally, it’s recommended that individuals work with a mental health professional to develop a comprehensive treatment plan that addresses their specific needs and goals.
Conclusion
In conclusion, it is clear that there is a significant link between trauma and nightmare frequency. Trauma can have a severe impact on an individual’s sleep patterns, leading to an increase in the occurrence of nightmares.
Understanding the science behind nightmares and the role of REM sleep helps us to comprehend why trauma can cause such disturbances. By disrupting the natural sleep cycle and impacting the regulation of emotions, trauma can provoke terrifying nightmares that can leave an individual feeling helpless and fearful.
Moreover, different types of trauma, such as physical assault or sexual abuse, can contribute to a higher incidence of nightmares. Additionally, prolonged trauma can lead to mental health conditions such as PTSD, which can further exacerbate nightmares.
However, there are treatment options and coping strategies available for managing trauma-related nightmares. These include seeking professional help from a therapist or counselor, making lifestyle changes such as exercise and relaxation techniques and developing coping mechanisms such as practicing mindfulness.
It is important to recognize that while nightmares can be distressing and debilitating, individuals can take proactive steps to manage them. Support from healthcare professionals, family, and friends can be invaluable in the recovery process.
In conclusion, by understanding the link between trauma and nightmares, we can work towards developing solutions that enable individuals to live healthier and happier lives.
Frequently Asked Questions
What are some common types of trauma that can lead to nightmares?
Some common types of trauma that can lead to nightmares include physical, emotional, or sexual abuse, experiencing or witnessing violence, natural disasters, and serious accidents.
Can trauma-related nightmares be treated?
Yes, there are treatments available such as therapy, medication, and lifestyle changes that can help manage trauma-related nightmares.
What is REM sleep?
REM (Rapid Eye Movement) sleep is a stage of sleep in which the brain is very active and dreaming occurs. It is also the stage of sleep during which nightmares typically occur.
Do all people who experience trauma develop nightmares?
No, not all people who experience trauma develop nightmares. However, it is a common symptom for those who have experienced trauma.
What is Post Traumatic Stress Disorder?
Post Traumatic Stress Disorder (PTSD) is a mental health disorder that can develop after experiencing or witnessing a traumatic event. Symptoms can include flashbacks, nightmares, anxiety, and avoidance of triggers related to the event.
Can nightmares be a symptom of other mental health disorders?
Yes, nightmares can be a symptom of other mental health disorders such as depression, anxiety, and sleep disorders.
Can lifestyle changes help manage trauma-related nightmares?
Yes, lifestyle changes such as regular exercise, healthy sleep habits, and reducing alcohol and drug use can help manage trauma-related nightmares.
What role do psychological mechanisms play in the link between trauma and nightmares?
Psychological mechanisms such as avoidance, hyperarousal, and negative interpretations of events can exacerbate the link between trauma and nightmares.
What is Cognitive Behavioral Therapy?
Cognitive Behavioral Therapy (CBT) is a type of therapy that focuses on changing negative thoughts, emotions, and behaviors. It has been shown to be effective in managing trauma-related nightmares.
Are there any medications that can help manage trauma-related nightmares?
Yes, there are medications such as Prazosin and some antidepressants that have been shown to help manage trauma-related nightmares.