Have you ever woken up in the middle of the night not being able to move or speak? It’s a terrifying experience that can leave you feeling confused and helpless. This phenomenon is known as sleep paralysis and it affects millions of people around the world. What causes sleep paralysis and how can we prevent it? Research has shown that underlying medical conditions may be linked to this mysterious disorder. In this article, we will explore the different types and causes of sleep paralysis, and how certain medical conditions may be contributing factors. So, let’s dive into the world of sleep paralysis and see what secrets it holds.
What is Sleep Paralysis?
Sleep paralysis is a perplexing phenomenon that affects many people around the world. During an episode of sleep paralysis, a person may be aware of their surroundings, but they are unable to move or speak. This can be an incredibly frightening experience, leaving individuals feeling helpless and vulnerable. The exact cause of sleep paralysis is not entirely clear, and there are a variety of factors that may contribute to its development. In the following sections, we will explore the symptoms, causes, and types of sleep paralysis in more detail.
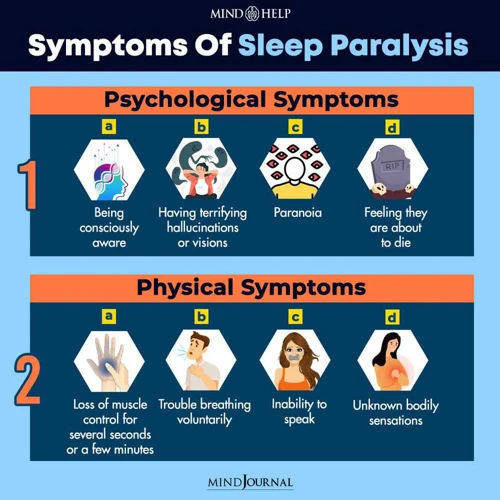
Symptoms of Sleep Paralysis
Sleep paralysis is a phenomenon that occurs when a person is unable to move or speak while transitioning between waking and sleeping states. This temporary inability to move or speak can be accompanied by some troubling symptoms, such as:
| Hallucinations | A sensation of seeing or hearing things that are not actually there. This can be a frightening experience, as the person may feel as though there is a presence in the room with them. |
| Feelings of pressure or choking | Some people experience a sense of pressure on their chest, as if someone or something is sitting on them. Others may feel as though they are being choked or strangled. |
| Feelings of fear or dread | Many people report feeling an intense sense of fear or dread during episodes of sleep paralysis, likely due to the hallucinations and feelings of pressure. |
| Rapid heart rate | Sleep paralysis can cause an increase in heart rate, which can contribute to the feelings of fear and panic. |
It is important to note that while sleep paralysis can be a disturbing experience, it is usually harmless and does not pose any physical harm to the person experiencing it. However, recurring episodes of sleep paralysis can lead to anxiety and disrupt one’s quality of sleep.
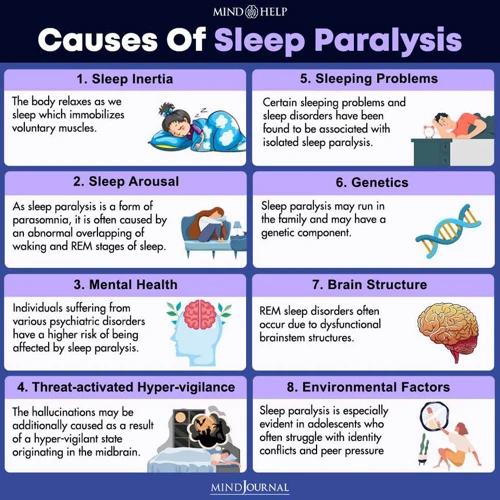
Causes of Sleep Paralysis
Sleep paralysis is a condition that occurs when a person is unable to move or speak upon waking up or falling asleep. There are several potential causes of sleep paralysis, including:
| Cause | Description |
|---|---|
| Disrupted sleep patterns | Sleep deprivation, irregular sleep schedules or jet lag can disrupt the normal sleep cycle, leading to potential episodes of sleep paralysis. |
| REM sleep dysregulation | Sleep paralysis can occur when the REM sleep cycle is disrupted, or when the brain does not properly regulate the neurotransmitters responsible for inhibiting muscle movement during REM sleep. |
| Stress and anxiety | High levels of stress or anxiety can also cause sleep paralysis, as the body may be unable to fully relax during sleep. |
| Genetics | Some individuals may have a genetic predisposition to sleep paralysis or certain underlying sleep disorders. |
| Underlying medical conditions | Sleep paralysis can also be a symptom of underlying medical conditions such as narcolepsy, sleep apnea, PTSD, and migraines, as well as neurological disorders including multiple sclerosis and Parkinson’s disease. |
It’s important to note that not all individuals who experience sleep paralysis have an underlying medical condition, and the condition may be brought on by a combination of factors. Understanding the potential causes of sleep paralysis is an important step in developing effective treatment strategies.
Types of Sleep Paralysis
Sleep paralysis is a relatively common phenomenon that is categorized into two types: isolated sleep paralysis and familiar sleep paralysis.
Isolated sleep paralysis is a type of sleep paralysis that occurs in individuals with no family history of the condition. It typically occurs during the transition between wakefulness and sleep stages. During this type of sleep paralysis, the person is unable to move, speak or react while fully conscious of their surroundings. The episodes are typically short-lived, lasting only a few seconds to several minutes.
Familiar sleep paralysis, on the other hand, is a type of sleep paralysis that occurs in individuals with a family history of sleep paralysis. It tends to be more frequent and severe than isolated sleep paralysis. During familiar sleep paralysis, the individual experiences the same symptoms as isolated sleep paralysis but may also experience hypnagogic hallucinations, vivid dreams that occur during the onset of sleep paralysis.
While understanding the types of sleep paralysis can provide some insight into the nature of the condition, it’s also important to note that sleep paralysis can occur as a symptom of underlying medical conditions. Understanding these underlying medical conditions and their connection to sleep paralysis is crucial in effectively treating and managing this condition.
Underlying Medical Conditions Linked to Sleep Paralysis
As we continue our journey to unlock the mysteries of dreaming, it’s important to examine the possible underlying medical conditions that can lead to sleep paralysis. Sleep paralysis is a phenomenon that affects a significant number of people, leaving them feeling trapped and unable to move or speak during sleep. It can be a terrifying experience, but identifying the medical conditions that can cause it can bring us one step closer to finding effective solutions. Let’s explore some of the medical conditions that have been linked to this phenomenon.
1. Narcolepsy
One of the underlying medical conditions that can lead to sleep paralysis is narcolepsy. This is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. People with narcolepsy may experience excessive daytime sleepiness, sudden and uncontrollable episodes of falling asleep, and changes in muscle control.
Symptoms of narcolepsy:
- Excessive daytime sleepiness
- Sudden and uncontrollable episodes of falling asleep
- Loss of muscle control or tone, called cataplexy, which may cause weakness, paralysis, and collapse
- Sleep paralysis
- Hypnagogic hallucinations, which are vivid and often frightening hallucinations that occur while falling asleep or waking up
Causes of narcolepsy:
The exact cause of narcolepsy is not known, but it is believed to involve abnormalities in certain brain chemicals and genetic factors. In some cases, narcolepsy may be triggered by an infection or a head injury.
Treatment of narcolepsy:
Although there is no cure for narcolepsy, medications and lifestyle changes can help manage the symptoms. Stimulants can help combat excessive daytime sleepiness, while antidepressants and other medications can help control cataplexy and hypnagogic hallucinations. Improving sleep habits and practicing good sleep hygiene can help manage symptoms and improve overall quality of life.
Conclusion:
Narcolepsy is a neurological disorder that can lead to a number of symptoms, including sleep paralysis. The condition is not fully understood, but treatment is available to help manage the symptoms and improve quality of life. If you’re experiencing symptoms of narcolepsy, it’s important to talk to your doctor for an accurate diagnosis and appropriate treatment plan.
2. Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA) is a sleep disorder characterized by breathing interruptions during sleep due to a complete or partial obstruction of the airway. This can lead to sleep paralysis, as well as other serious health issues.
What are the symptoms of OSA?
– Loud snoring
– Choking or gasping during sleep
– Daytime sleepiness
– Morning headache
– Difficulty concentrating
– Irritability or mood changes
What causes OSA?
OSA is often caused by excess weight, due to the fat deposits around the neck and throat that can obstruct breathing. However, other risk factors include:
– Being male
– Being over the age of 40
– Having a family history of OSA
– Having a large tongue or tonsils
– Smoking or alcohol consumption
How is OSA treated?
Treatment for OSA typically involves lifestyle changes, such as losing weight and avoiding alcohol and smoking. Additionally, devices such as continuous positive airway pressure (CPAP) machines may be used to keep the airway open during sleep. In severe cases, surgery may be necessary to remove excess tissue from the throat or reposition the jaw.
If you suspect that you may have OSA or experience symptoms of sleep paralysis, it is important to talk to your doctor about proper diagnosis and treatment options.
3. Rapid Eye Movement (REM) Sleep Behavior Disorder
Rapid Eye Movement (REM) Sleep Behavior Disorder (RBD) is a neurological condition that occurs during the REM stage of sleep. This sleep disorder is characterized by disturbing dreams that lead to alarming physical movements during sleep. During REM sleep, our muscles become paralyzed, but in individuals with RBD their muscles remain active, causing them to act out their dreams. This can lead to various physical injuries.
Symptoms: The primary symptom of RBD is acting out vivid and often violent dreams during sleep. These dreams may involve physically demanding activities like running, jumping, or even punching. Individuals with RBD may also talk, shout, or scream during sleep. Additionally, they may experience injuries such as bruises or even broken bones due to these movements.
Causes: RBD is caused by the malfunctioning of the neurons that are responsible for inhibiting muscle movement during REM sleep. The exact cause of this malfunction is not fully understood, but it is thought to be linked to underlying neurological conditions such as Parkinson’s disease or multiple system atrophy.
Treatment: Treatment for RBD involves addressing any underlying neurological conditions and medications such as clonazepam, melatonin, or antidepressants to help mitigate symptoms. It’s also recommended to create a safe sleep environment to prevent injuries during sleep.
| Symptoms | Causes | Treatment |
|---|---|---|
| Acting out vivid and often violent dreams during sleep | Malfunctioning of the neurons that inhibit muscle movement during REM sleep; likely related to neurological conditions | Address underlying conditions; medication such as clonazepam, melatonin, or antidepressants; create a safe sleep environment |
| Movement during sleep resulting in injuries such as bruises or even broken bones |
If you suspect you may have RBD, it’s important to talk to your doctor. They may refer you to a sleep specialist for further evaluation and treatment.
4. Anxiety Disorders
Anxiety disorders are another medical condition that can lead to sleep paralysis. This condition affects millions of people worldwide, causing them to experience a range of symptoms, including persistent and excessive worry, fear, and apprehension. Here are some of the specific anxiety disorders that have been linked to sleep paralysis:
- Generalized Anxiety Disorder (GAD): GAD is a common anxiety disorder marked by persistent and excessive worries about everyday events and activities. Studies have shown that people with GAD are more likely to experience insomnia and other sleep disorders, including sleep paralysis.
- Panic Disorder: Panic disorder is an anxiety disorder marked by sudden and repeated panic attacks – periods of intense fear or discomfort that peak within minutes. People with panic disorder may also experience sleep disturbances, including sleep paralysis.
- Social Anxiety Disorder: Also known as social phobia, this anxiety disorder is characterized by intense fear or discomfort in social situations. People with social anxiety disorder may avoid social situations altogether, leading to social isolation, depression and other mental health problems. Studies have shown that social anxiety disorder is associated with a higher risk of sleep disturbances, including sleep paralysis.
While it’s not entirely clear why anxiety disorders can lead to sleep paralysis, researchers believe that the disruptions in the normal sleep cycle, which is controlled by the brain, may play a role. Anxiety can also cause muscle tension and make it difficult to relax, which can contribute to sleep paralysis.
If you suffer from an anxiety disorder and have symptoms of sleep paralysis, it’s important to seek medical help. A healthcare professional can evaluate your symptoms, recommend a treatment plan, and work with you to manage your condition effectively. Some of the treatment options may include medication, talk therapy, stress reduction techniques and good sleep habits.
5. Post-traumatic Stress Disorder (PTSD)
The fifth underlying medical condition that has been linked to sleep paralysis is Post-traumatic Stress Disorder (PTSD). PTSD is a mental health condition that often develops after a person has experienced or witnessed a traumatic event. In PTSD, the brain’s response to stress is altered, leading to symptoms such as flashbacks, nightmares, and intense feelings of anxiety.
PTSD has been linked to sleep paralysis, as both conditions affect the rapid eye movement (REM) stage of sleep. In particular, individuals with PTSD may experience more frequent and intense episodes of sleep paralysis due to disruptions in their REM sleep.
Studies have shown that individuals with PTSD have a higher prevalence of sleep paralysis compared to the general population. One study found that nearly 30% of individuals with PTSD reported experiencing sleep paralysis, compared to only 7% of individuals without PTSD.
Interestingly, some research suggests that treating PTSD symptoms may also help alleviate sleep paralysis. In a study of individuals with PTSD-related sleep paralysis, those who received cognitive behavioral therapy (CBT) for their PTSD symptoms saw a significant reduction in the frequency and severity of their sleep paralysis episodes.
It is important for individuals with PTSD to address their sleep paralysis symptoms with their healthcare provider, as treatment for PTSD may also improve their sleep paralysis symptoms. Additionally, practicing good sleep hygiene and stress-reduction techniques may also be helpful for managing sleep paralysis in individuals with PTSD.
| Post-traumatic Stress Disorder (PTSD) |
|---|
| PTSD often develops after a person has experienced or witnessed a traumatic event. |
| PTSD alters the brain’s response to stress. |
| Symptoms of PTSD include flashbacks, nightmares, and intense anxiety. |
| Individuals with PTSD may experience more frequent and intense episodes of sleep paralysis due to disruptions in their REM sleep. |
| Nearly 30% of individuals with PTSD reported experiencing sleep paralysis, compared to only 7% of individuals without PTSD. |
| Treatment for PTSD may also alleviate sleep paralysis symptoms. CBT has shown to be effective in reducing frequency and severity of sleep paralysis episodes. |
| Practicing good sleep hygiene and stress-reduction techniques may also be helpful for managing sleep paralysis in individuals with PTSD. |
6. Migraine Headaches
Migraine headaches, a common condition affecting millions of people worldwide, have been linked to sleep paralysis in some individuals. During a migraine attack, a person may experience intense throbbing pain on one side of the head, along with nausea, dizziness, and sensitivity to light and sound.
The link between migraine headaches and sleep paralysis may be due to the disruption of normal sleep patterns. Migraine sufferers often have difficulty falling asleep and staying asleep due to the pain and other symptoms associated with the condition. This can lead to sleep deprivation and a higher likelihood of experiencing sleep paralysis.
Additionally, migraines can trigger changes in neurotransmitters and brain activity that may lead to sleep paralysis. During a migraine attack, the levels of certain neurotransmitters in the brain, such as serotonin and dopamine, can fluctuate. These changes in neurotransmitter levels can alter brain activity in ways that may make sleep paralysis more likely.
To manage sleep paralysis associated with migraines, it is important to manage migraine symptoms and improve sleep habits. Migraine sufferers should work with their healthcare provider to develop a treatment plan that effectively manages their symptoms, which may include medications, stress-reduction techniques, and lifestyle modifications. Additionally, maintaining a regular sleep schedule and practicing good sleep hygiene can help reduce the likelihood of experiencing sleep paralysis.
7. Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is a neurological disorder that affects the central nervous system. MS can cause a variety of symptoms, including vision problems, muscle weakness, and difficulty with coordination and balance. Sleep paralysis is another symptom that has been associated with MS.
Research suggests that as many as 40% of people with MS experience sleep disturbances, including sleep paralysis. This can be due to the damage that MS causes to the myelin sheaths that surround nerve fibers in the brain and spinal cord, which can disrupt the normal functioning of the central nervous system.
Studies have found that the prevalence of sleep paralysis in people with MS is higher than in the general population. One study published in the journal Clinical Neuropsychology found that nearly 30% of people with MS experienced sleep paralysis compared to just 7% of healthy controls.
Table:
| MS and Sleep Paralysis | Prevalence |
|---|---|
| MS patients who experience sleep paralysis | ~30% |
| Healthy controls who experience sleep paralysis | ~7% |
It is important for people with MS who are experiencing sleep paralysis to discuss their symptoms with their healthcare provider. Treatment options may include medications for MS and sleep disturbances, as well as lifestyle changes and stress management techniques. It is also important for individuals with MS to maintain good sleep hygiene and follow a regular sleep schedule to reduce the occurrence of sleep paralysis and other sleep disturbances.
8. Parkinson’s Disease (PD)
Parkinson’s disease (PD) is a chronic neurological disorder that affects movement. It occurs when neurons in the brain, which produce a chemical called dopamine, begin to die off. Dopamine helps to control movement and coordination, so as the brain loses dopamine-producing neurons, it becomes more difficult for a person to move their muscles.
People with PD often experience sleep disturbances, including sleep paralysis. A study published in the Journal of Neurology, Neurosurgery & Psychiatry found that sleep paralysis was present in over half of PD patients, compared to only a third of people without PD.
The exact cause of sleep paralysis in PD is still unknown. However, it is thought to be related to changes in the brain that occur as a result of the disease. During REM sleep, the brainstem normally inhibits muscle movement, allowing a person to remain still while they dream. In PD, this inhibition may be altered, leading to episodes of sleep paralysis.
In addition to sleep paralysis, PD can also cause other sleep-related disorders, such as restless leg syndrome and REM sleep behavior disorder. These disorders can disrupt a person’s sleep and cause them to feel tired and fatigued during the day, which can further exacerbate their Parkinson’s symptoms.
Treatment for sleep paralysis in PD typically involves addressing the underlying Parkinson’s disease. This may include taking medications to increase dopamine levels in the brain, engaging in regular exercise to improve muscle coordination, and practicing good sleep hygiene to reduce the risk of sleep disturbances.
Table:
Medical Condition | Characteristics
— | —
Parkinson’s disease (PD) | Neurological disorder that affects movement due to the death of dopamine-producing neurons in the brain.
Sleep paralysis in PD | Present in over half of PD patients, compared to only a third of people without PD.
Cause of sleep paralysis in PD | Thought to be related to changes in the brain that occur as a result of the disease, which alter the brainstem’s inhibition of muscle movement during REM sleep.
Other sleep-related disorders in PD | Restless leg syndrome and REM sleep behavior disorder, which can disrupt a person’s sleep and worsen Parkinson’s symptoms.
Treatment for sleep paralysis in PD | Involves addressing the underlying Parkinson’s disease with medications, exercise, and good sleep hygiene.
How to Handle Sleep Paralysis
After experiencing a terrifying episode of sleep paralysis, it’s natural to feel confused and overwhelmed. The good news is that there are several steps you can take to prevent future episodes or make them less severe. By implementing some simple lifestyle changes and seeking medical help, you can learn to handle sleep paralysis and reduce its impact on your life. Let’s take a closer look at some effective strategies for managing sleep paralysis.
1. Improve Your Sleep Habits
Improving your sleep habits is one of the most effective ways to tackle sleep paralysis. Here are some simple yet effective tips you can follow to improve your sleep:
- Stick to a sleep schedule: Try to go to bed and wake up at the same time every day, including weekends. This helps regulate your body’s internal clock and improves the quality of your sleep.
- Create a sleep-conducive environment: Make sure your bedroom is comfortable, quiet, and cool. Keep the room dark with the help of blackout curtains, or wear an eye mask if necessary. Make sure your bed and pillows are comfortable.
- Avoid stimulating activities before bedtime: Exercising, watching TV, or using electronic devices before bedtime can disrupt your sleep. Instead, try relaxing activities like reading a book or taking a warm bath.
- Avoid caffeine and alcohol: Caffeine and alcohol can interfere with your sleep. Try to avoid consuming them for at least several hours before bedtime.
- Don’t eat heavy meals close to bedtime: Eating a heavy or spicy meal close to bedtime can cause indigestion and disrupt your sleep.
- Limit your exposure to light: Exposure to bright light, especially blue light from electronic devices, can interfere with your sleep. Try to limit your exposure to light for at least an hour before bedtime.
- Stay relaxed: If you feel anxious or stressed before bedtime, try relaxation techniques like deep breathing or meditation to calm your mind.
Improving your sleep habits may take time and effort, but it can greatly improve the quality of your sleep and reduce the frequency of sleep paralysis.
2. Address Medical Conditions
Addressing underlying medical conditions is key to preventing sleep paralysis. Identifying the medical conditions and seeking treatment can help reduce the frequency and intensity of episodes. Here are some medical conditions associated with sleep paralysis and ways to address them:
- Narcolepsy: This is a neurological disorder that causes excessive daytime sleepiness and sudden attacks of sleep. Treating narcolepsy with medications, such as stimulants, can help improve symptoms and reduce the occurrence of sleep paralysis.
- Obstructive Sleep Apnea (OSA): This is a sleep disorder characterized by loud snoring and interrupted breathing during sleep. Treating OSA with continuous positive airway pressure (CPAP) machines can improve breathing and reduce the likelihood of sleep paralysis.
- Rapid Eye Movement (REM) Sleep Behavior Disorder: This is a sleep disorder where the body does not enter paralysis during REM sleep, resulting in acting out of dreams. Treating REM sleep behavior disorder with medications, such as clonazepam, can help reduce the occurrence of sleep paralysis.
- Anxiety Disorders: Anxiety disorders, such as panic disorder and generalized anxiety disorder, can affect sleep and increase the risk of sleep paralysis. Treating anxiety disorders with therapy or medication, such as benzodiazepines, can help reduce anxiety and improve sleep quality.
- Post-traumatic Stress Disorder (PTSD): PTSD can cause nightmares and disrupted sleep, leading to an increased risk of sleep paralysis. Treating PTSD with therapy, medication, or both can help reduce the occurrence of sleep paralysis.
- Migraine Headaches: Migraine headaches can disrupt sleep and increase the risk of sleep paralysis. Treating migraines with medications, such as triptans, can help reduce the frequency of migraines and improve sleep quality.
- Multiple Sclerosis (MS): MS can cause sleep disturbances and increase the risk of sleep paralysis. Treating MS with medication, such as disease-modifying therapies or muscle relaxants, can help reduce symptoms and improve sleep quality.
- Parkinson’s Disease (PD): PD can cause sleep disturbances, such as restless leg syndrome, and increase the risk of sleep paralysis. Treating PD with medication, such as levodopa, can help improve symptoms and reduce the risk of sleep paralysis.
It’s important to consult with a doctor to properly diagnose and treat any medical conditions that may be contributing to sleep paralysis. Addressing these underlying medical conditions can greatly improve sleep quality and reduce the occurrence of sleep paralysis.
3. Practice Stress-Reduction Techniques
It’s important to note that stress can be a major factor in sleep paralysis. Practicing stress-reduction techniques can be a helpful way to reduce the likelihood of experiencing sleep paralysis. Here are some tips for practicing stress reduction:
- Meditation: Meditation is a technique that involves focusing your attention on a specific object, thought, or activity to help clear your mind and reduce stress. This practice has been shown to be effective in reducing the symptoms of sleep disorders in several studies.
- Yoga: Yoga is a form of exercise that combines physical poses, breathing techniques, and meditation to help relax and reduce stress. Practicing yoga regularly can improve not only your physical health but also your mental health.
- Deep breathing exercises: Deep breathing is a practice that involves taking slow, deep breaths in through your nose, and then releasing the air slowly through your mouth. This can help you relax and calm down, which can be helpful when trying to combat stress and anxiety.
- Progressive muscle relaxation: This technique involves tensing and then relaxing different muscle groups throughout your body, which can help release tension and reduce stress. This method can also help improve your overall sleep quality.
- Cognitive-behavioral therapy (CBT): CBT is a form of talk therapy that can help you identify and change negative thoughts and behaviors that may be contributing to your stress levels. It has been shown to be effective in treating a variety of mental health conditions, including anxiety and depression.
It’s important to find a stress-reduction technique that works for you and to practice it regularly in order to see the benefits.
4. Talk to Your Doctor About Medications
If improving sleep habits and addressing underlying medical conditions do not alleviate sleep paralysis, it may be time to talk to a doctor about medications that can help manage the symptoms. There are a few different types of medications that can be prescribed for sleep paralysis, so it’s important to work with a healthcare professional to determine the best course of action.
1. Antidepressants: Selective Serotonin Reuptake Inhibitors (SSRIs) and Tricyclic Antidepressants (TCAs) are commonly prescribed to help manage the symptoms of sleep paralysis. These medications can help regulate serotonin levels in the brain, which can improve sleep quality and reduce the frequency and intensity of sleep paralysis episodes.
2. Benzodiazepines: These medications, like diazepam and clonazepam, are often prescribed to help with anxiety and can also help manage the symptoms of sleep paralysis. Benzodiazepines can help calm the mind and body, which can prevent or reduce the severity of episodes.
3. Anti-anxiety medications: Medications like buspirone and gabapentin can help manage anxiety, which can be a trigger for sleep paralysis. These medications can also promote relaxation and reduce muscle tension, which can help prevent episodes.
It’s important to note that medications should only be taken under the guidance of a healthcare professional, as they can have side effects and risks. Additionally, medication should not be considered the only solution for managing sleep paralysis, but rather a complementary strategy to be used in conjunction with other measures, such as improved sleep habits and addressing underlying medical conditions.
Conclusion
In closing, it is important to understand that sleep paralysis is a common and frightening experience that affects a significant portion of the population. The root cause of this condition can vary widely, from poor sleep habits to underlying medical conditions.
If you are experiencing sleep paralysis, it is essential to seek the guidance of a healthcare professional to ensure that you receive the proper diagnosis and treatment. Through a combination of improved sleep hygiene, stress-reduction techniques, medical intervention, and lifestyle changes, you can effectively manage and overcome sleep paralysis symptoms.
Remember that while sleep paralysis can be a challenging and distressing experience, it is ultimately a treatable condition. By taking the necessary steps to manage your symptoms, you can enjoy a more restful and peaceful night’s sleep, free from the terrors of sleep paralysis.
Don’t let sleep paralysis control your life. Seek help and take control of your sleep health today.
Frequently Asked Questions
What is the difference between sleep paralysis and nightmares?
Sleep paralysis involves the inability to move or speak during a transition between awake and sleep. Nightmares are terrifying dreams with various themes that elicit fear, anxiety, or sadness.
Is sleep paralysis common?
It is estimated that about 8% of people experience sleep paralysis at some point in their lives. It can occur in healthy individuals as well as those with underlying medical conditions.
Can sleep paralysis be dangerous?
Sleep paralysis itself is not dangerous, but it can be a symptom of underlying medical conditions that require treatment. Additionally, some people may experience significant stress and anxiety from sleep paralysis episodes.
Can children experience sleep paralysis?
Yes, children can experience sleep paralysis, although it is not as common as in adults. It typically occurs in adolescence and young adulthood.
Can changing sleep positions prevent sleep paralysis?
Changing sleep positions may reduce the frequency of sleep paralysis episodes, but it is not a guarantee. Improving overall sleep habits, including getting regular and sufficient sleep, can also help minimize episodes.
Can medication cause sleep paralysis?
Some medications, particularly those that affect the sleep cycle, can potentially contribute to sleep paralysis. However, it is important to consult with your doctor and consider other factors before making a determination.
Is there a cure for sleep paralysis?
There is no known cure for sleep paralysis, but addressing any underlying medical conditions and improving sleep habits can reduce the frequency and severity of episodes.
Can sleep paralysis be a sign of a serious medical condition?
Sleep paralysis can be a symptom of underlying medical conditions, including narcolepsy, sleep apnea, and post-traumatic stress disorder. Discussing symptoms with a doctor can help identify any serious medical conditions.
Are there any home remedies for sleep paralysis?
While there are no proven home remedies for sleep paralysis, relaxation techniques and stress-reduction practices may help minimize episodes.
What should you do if you experience frequent sleep paralysis?
If sleep paralysis is happening frequently and causing significant stress or fear, it may be a good idea to discuss symptoms with a doctor. They can help identify any underlying medical conditions and suggest treatment options.