As we lay in bed at night, our brains continue to work, producing dreams that can be both vivid and bizarre. Many of us may toss and turn or even talk in our sleep without realizing it. However, for some individuals, these behaviors can escalate into more serious issues, such as REM sleep behavior disorder. Despite being a well-known condition, the causes and risk factors of REM sleep behavior disorder remain somewhat of a mystery. In this article, we’ll explore the possible causes and risk factors that can contribute to REM sleep behavior disorder, and what can be done to treat and possibly prevent it.
Definition of REM Sleep Behavior Disorder

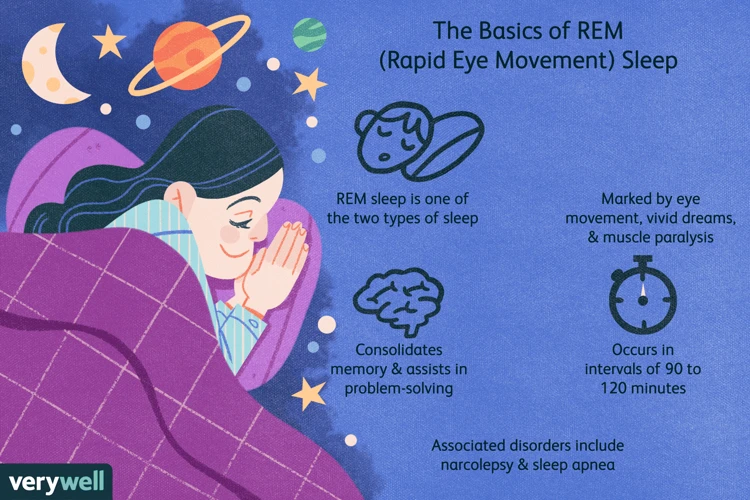
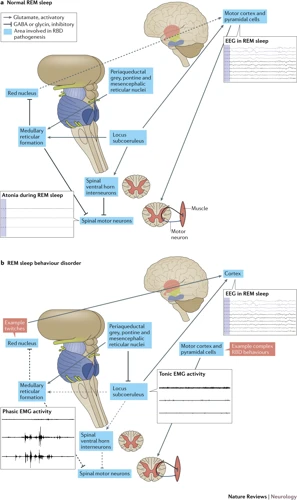
During sleep, our body goes through different stages of sleep. One of these stages is the Rapid Eye Movement (REM) sleep, which is characterized by increased brain activity and rapid eye movements. In REM sleep behavior disorder (RBD), the body doesn’t stay still during REM sleep, unlike a normal person whose muscles relax and paralyze during the period. Instead, people with RBD act out their dreams physically, sometimes violently, and can even injure themselves or their partners.
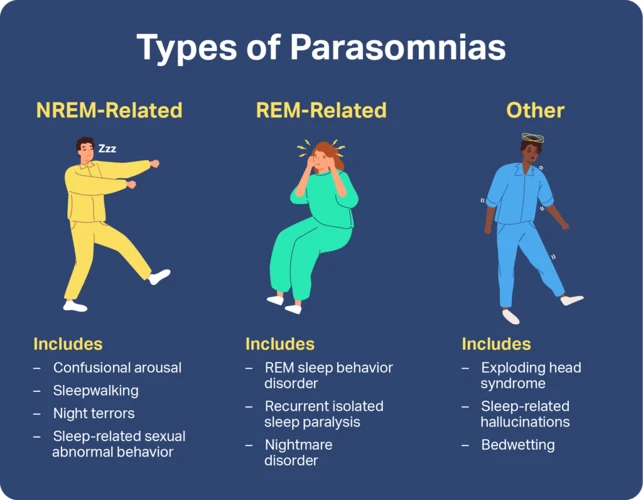
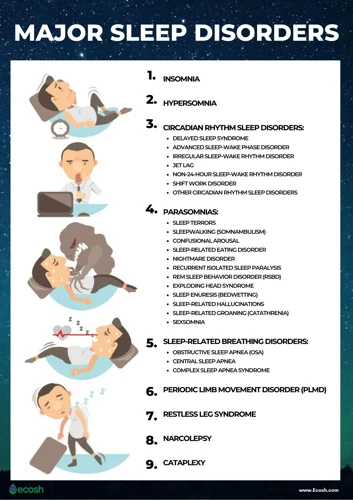
RBD is classified as a parasomnia, a type of sleep disorder where abnormal behaviors, movements, or experiences occur during sleep. It was first described in 1986 and recognized as a clinical disorder in the 2005 edition of the International Classification of Sleep Disorders. RBD is often associated with other neurological and psychiatric disorders, but it can also occur in otherwise healthy individuals.
The exact prevalence of RBD is unknown since it often goes undiagnosed or misdiagnosed. It is more common in men than women and tends to occur in middle-aged or elderly people. RBD can be a precursor to certain neurodegenerative diseases, such as Parkinson’s disease, dementia with Lewy bodies, and multiple system atrophy, and sometimes is a symptom of these diseases.
Causes of REM Sleep Behavior Disorder
The precise causes of REM Sleep Behavior Disorder (RBD) remain largely puzzling to the medical community. Researchers have identified several factors that may lead to the development of RBD. Despite significant advances in sleep medicine, the exact mechanisms that trigger RBD are not yet fully understood. However, there is growing empirical evidence to suggest that several factors, such as neurodegenerative diseases, genetics, and certain medications, can increase the risk of developing RBD. Let’s delve into each of these factors in detail to get a comprehensive understanding of the causes of this sleep disorder.
1. Neurodegenerative Diseases
One of the primary causes of REM Sleep Behavior Disorder (RBD) is neurodegenerative diseases, which cause damage to the brain and nerves responsible for regulating sleep. Some examples of neurodegenerative diseases that can lead to RBD include Parkinson’s disease, multiple system atrophy, and dementia with Lewy bodies.
These diseases are characterized by the progressive loss of function of nerve cells in certain areas of the brain, which can ultimately lead to the development of RBD. In some cases, RBD may be an early sign of a neurodegenerative disease, even before other symptoms emerge.
In Parkinson’s disease, for instance, there is a depletion of dopamine, a chemical in the brain that influences movement and other functions. This depletion can disrupt the normal functioning of the parts of the brain involved in sleep regulation, leading to RBD. Similarly, in multiple system atrophy, a rare disorder that affects the nervous system, damage to the nerves can interfere with the brain’s control of the body during sleep, resulting in RBD.
While the exact mechanisms through which neurodegenerative diseases cause RBD are not fully understood, it is believed that the loss of nerve cells and the associated changes in brain chemistry disrupt the body’s normal sleep patterns, leading to abnormal behaviors during REM sleep. It is important to note that not everyone with a neurodegenerative disease will develop RBD, and not everyone with RBD will go on to develop a neurodegenerative disease. However, RBD can be a warning sign of an underlying neurological condition, and anyone experiencing symptoms of RBD should seek medical attention.
To summarize, neurodegenerative diseases are one of the primary causes of REM Sleep Behavior Disorder, and can lead to disruptions in the body’s normal sleep patterns. Diseases like Parkinson’s, multiple system atrophy, and dementia with Lewy bodies all have the potential to cause RBD, which can be an early warning sign of an underlying neurological condition. It is important for individuals who experience symptoms of RBD to seek a medical evaluation to determine the underlying cause and appropriate treatment.
2. Genetics
Several studies have shown that genetics can play a significant role in the development of REM Sleep Behavior Disorder (RBD). In fact, it has been suggested that people who have a family history of RBD may be at a higher risk of developing the disorder themselves.
One study found that individuals with first-degree relatives who had RBD were more likely to exhibit RBD-like behaviors during sleep. The study also identified a specific genetic mutation that was more prevalent in people with RBD than in the general population.
Researchers have identified a gene known as glutamate decarboxylase 1 (GAD1) that may be associated with an increased risk of RBD. GAD1 is involved in the regulation of the neurotransmitter gamma-aminobutyric acid (GABA), which is thought to play a role in REM sleep.
It is important to note that having a particular genetic mutation or variant does not necessarily mean that an individual will develop RBD. Other environmental and lifestyle factors may also contribute to the development of the disorder.
The following table summarizes some of the key genetic factors that have been implicated in RBD:
| Gene | Function | Association with RBD |
|---|---|---|
| Glutamate decarboxylase 1 (GAD1) | Regulation of GABA neurotransmitter | Increased risk |
| Leucine-rich repeat kinase 2 (LRRK2) | Enzyme involved in cellular signaling | Increased risk (in cases with Parkinson’s disease) |
| CATSPER2 | Ion channel involved in sperm function | May be involved in regulation of REM sleep |
While further research is needed to fully understand how genetics contributes to the development of RBD, it is clear that genetic factors play a significant role in the disorder. Anyone with a family history of RBD should talk to their doctor to determine if they may be at an increased risk of developing the disorder themselves.
3. Medications and Substances
Certain medications and substances can contribute to the development of REM sleep behavior disorder (RBD), either by triggering its onset or exacerbating existing symptoms. Here are some examples:
- Antidepressants: Certain antidepressants known as selective serotonin reuptake inhibitors (SSRIs) have been linked to an increased risk of RBD. These include fluoxetine, paroxetine, and sertraline. Tricyclic antidepressants such as amitriptyline and imipramine may also be associated with RBD.
- Antipsychotics: Drugs used to treat schizophrenia and other psychiatric disorders, including haloperidol and olanzapine, have been known to cause RBD.
- Sedatives: Benzodiazepines such as diazepam and lorazepam, which are commonly used to treat anxiety and sleep disorders, can suppress REM sleep and lead to rebound RBD symptoms.
- Alcohol and recreational drugs: Alcohol and certain drugs such as cocaine and amphetamines can disrupt sleep and contribute to RBD.
It’s important to note that not everyone who takes these medications or uses these substances will develop RBD. However, individuals who have a history of RBD or other sleep disorders may be more susceptible to developing symptoms as a result of these factors. If you suspect that your medication or substance use may be contributing to RBD symptoms, it’s important to speak with your healthcare provider to discuss potential alternatives or adjustments to your treatment plan.
Risk Factors of REM Sleep Behavior Disorder
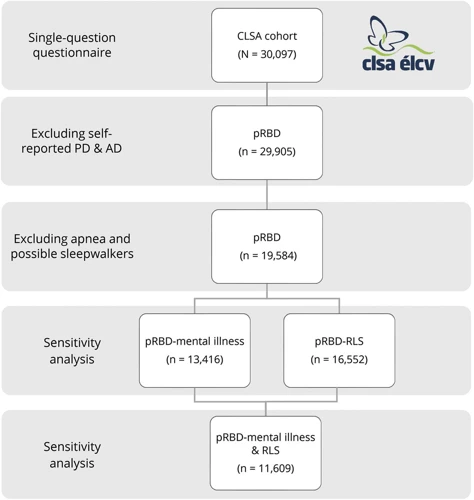
While the exact cause of REM Sleep Behavior Disorder (RBD) is not fully understood, there are certain factors that can increase an individual’s risk of developing this sleep disorder. RBD is often associated with other underlying conditions, including neurodegenerative diseases, which may lead to the development of the disorder. However, there are several additional risk factors that individuals need to be aware of. Understanding these risk factors and taking necessary precautions can ultimately prevent the onset of RBD or manage the symptoms effectively. In this section, we will explore some of the most significant risk factors associated with REM Sleep Behavior Disorder.
1. Gender and Age
Several risk factors have been identified for the development of REM Sleep Behavior Disorder (RBD), and one of the most significant ones is gender and age. Studies suggest that men are more prone to develop RBD than women. RBD is more commonly observed in older adults above 50 years of age.
Gender:
The reason behind the gender difference in RBD incidence is not entirely clear, but some researchers believe that it may be related to the fact that men and women have different sleep architecture. Men tend to have more REM sleep and less non-REM sleep than women, which may make them more vulnerable to RBD. Additionally, hormonal differences may play a role in this gender difference.
Age:
As for age, it is believed that RBD is associated with the aging process. As we age, the neurons in the brain responsible for regulating REM sleep become less efficient, which can lead to a disruption in the normal sleep process. This, in turn, can trigger the onset of RBD symptoms.
It is important to note that although men and older adults are at a higher risk of developing RBD, anyone can develop the condition. It is not uncommon for RBD to occur in younger individuals, especially those who have a family history of the disorder or have a history of head injuries. It is essential to be aware of the risk factors and recognize the symptoms of RBD, regardless of age and gender.
2. Other Sleep Disorders
REM sleep behavior disorder (RBD) is a condition in which people physically act out their dreams while they sleep. RBD can occur on its own or as a symptom of other sleep disorders. It is important to recognize other sleep disorders because they can contribute to RBD and impact the diagnosis and treatment.
Table: Common Sleep Disorders That Can Contribute to RBD
| Sleep Disorder | Description |
|---|---|
| Narcolepsy | A chronic neurological disorder that affects the brain’s ability to regulate wakefulness and sleep cycles. People with narcolepsy can experience sudden, uncontrollable sleep attacks during the day and can have vivid, intense dreams during REM sleep. |
| Obstructive Sleep Apnea (OSA) | A condition in which the air passage is partially or completely blocked during sleep, causing interrupted breathing and frequent awakenings. OSA can cause fluctuations in oxygen levels in the brain, which can trigger RBD. |
| Restless Leg Syndrome (RLS) | A neurological disorder characterized by an intense urge to move the legs during rest or sleep. People with RLS can experience involuntary leg movements during sleep, which may contribute to RBD. |
| Insomnia | A common sleep disorder characterized by difficulty falling or staying asleep. Insomnia can cause sleep fragmentation and lead to increased REM sleep, which can trigger RBD. |
Narcolepsy, obstructive sleep apnea (OSA), restless leg syndrome (RLS), and insomnia are all common sleep disorders that can contribute to RBD.
Narcolepsy, for example, is a chronic neurological disorder that affects the brain’s ability to regulate wakefulness and sleep cycles. People with narcolepsy can experience sudden, uncontrollable sleep attacks during the day and have vivid, intense dreams during REM sleep. These vivid dreams can make RBD more likely and common in people with narcolepsy.
OSA is a condition in which the air passage is partially or completely blocked during sleep, causing interrupted breathing and frequent awakenings. OSA can cause fluctuations in oxygen levels in the brain, which can trigger RBD.
RLS is a neurological disorder characterized by an intense urge to move the legs during rest or sleep. People with RLS can experience involuntary leg movements during sleep, which may contribute to RBD.
Insomnia, on the other hand, is a common sleep disorder characterized by difficulty falling or staying asleep. Insomnia can cause sleep fragmentation and lead to increased REM sleep, which can trigger RBD.
It is important for individuals experiencing symptoms of RBD to seek a proper diagnosis and treatment, especially if they are also dealing with other sleep-related disorders.
3. Mental Health Disorders
REM Sleep Behavior Disorder can also be linked to certain mental health disorders. People suffering from mental health disorders such as anxiety, depression, and post-traumatic stress disorder (PTSD) are more likely to experience REM Sleep Behavior Disorder. The link between these disorders and REM Sleep Behavior Disorder is not fully understood, but it is believed that the disrupted sleep patterns associated with these conditions can also influence the onset of REM Sleep Behavior Disorder.
Additionally, those suffering from psychotic disorders such as schizophrenia can also be at greater risk for developing REM Sleep Behavior Disorder. Studies have shown a correlation between psychotic symptoms and increased frequency and intensity of REM Sleep Behavior Disorder symptoms.
It is important to note that the link between mental health disorders and REM Sleep Behavior Disorder is still being studied and not fully understood. However, if you suffer from a mental health disorder and also experience symptoms of REM Sleep Behavior Disorder, it is important to speak with your healthcare provider to develop the best plan of action for managing your symptoms.
Symptoms of REM Sleep Behavior Disorder
REM Sleep Behavior Disorder (RBD) is characterized by abnormal and often violent behaviors during Rapid Eye Movement (REM) sleep. Individuals with RBD typically act out vivid and action-packed dreams, often screaming, kicking, and thrashing around in bed. Some common symptoms of RBD include:
1. Physical Movements: The most obvious symptom of RBD is the physical movements that occur during REM sleep. These movements can range from mild twitching to violent thrashing and kicking, which may result in injury to either the individual or their bed partner.
2. Verbalizations: Many people with RBD also exhibit loud and disruptive vocalizations during REM sleep. These vocalizations can include speaking, shouting, screaming, and even singing.
3. Acting Out Dreams: In RBD, individuals may act out their dreams, often in a violent or aggressive manner. This can lead to injuries to themselves or their sleep partner.
4. Emotional Disturbances: RBD can also cause emotional disturbances during sleep, such as laughing or crying in response to dreams.
5. Partial or Total Awakening: While individuals with RBD are technically asleep during these episodes, they may experience partial or total awakenings during or after the episode, causing daytime sleepiness and fatigue.
It’s important to note that not everyone who experiences physical movements during sleep has RBD, and a proper diagnosis is necessary.
Diagnosis of REM Sleep Behavior Disorder
Diagnosing REM Sleep Behavior Disorder (RBD) can be a complex process as it requires a detailed assessment of a patient’s sleep patterns and behavior during sleep. The diagnosis of RBD is primarily made based on a combination of a clinical and polysomnographic evaluation.
Clinical evaluation: The first step in diagnosing RBD is usually a detailed clinical evaluation. A doctor may ask questions about a patient’s medical history, including any medications they are taking, as well as questions about their sleep patterns and any unusual behaviors during sleep. It is important that the patient provides as much detail as possible about their experiences to help the doctor make an accurate diagnosis.
Polysomnography: Polysomnography is a sleep study that involves monitoring a patient’s sleep patterns, brain waves, heart rate, and breathing patterns during sleep. This test is typically conducted overnight in a sleep lab, where the patient is connected to electrodes that record the various physiological parameters. The test is used to rule out other sleep disorders and to confirm the presence of RBD.
Movement monitoring: A movement monitoring device, such as an accelerometer or a video monitor, may be used to record a patient’s movements during sleep. This can help to confirm the presence of RBD and to assess the severity of the disorder.
Neurological evaluation: In some cases, a neurological evaluation may be conducted to rule out other neurological conditions that can cause similar symptoms to RBD.
It is important to note that RBD can often be misdiagnosed, as the symptoms can be similar to other sleep disorders or medical conditions. It is important for patients to seek out a qualified sleep specialist who has experience evaluating patients with RBD.
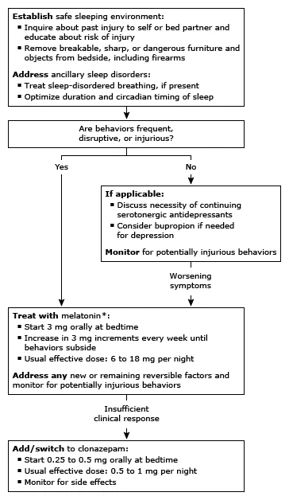
Treatment for REM Sleep Behavior Disorder

As with many sleep disorders, treating REM Sleep Behavior Disorder can be a complex and challenging process. There are various approaches for managing the symptoms of RBD, ranging from medications to lifestyle changes. While some treatments may be effective for some individuals with RBD, others may require a combination of therapies for optimal results. Let’s dive deeper into the available options for treating REM Sleep Behavior Disorder.
1. Medications
When it comes to treating REM Sleep Behavior Disorder, medications can be an effective option for managing symptoms. There are a few different types of medication that may be used, depending on the severity and underlying causes of the disorder.
Clonazepam is a medication that is commonly used to treat REM Sleep Behavior Disorder. It is a type of benzodiazepine, which means that it works by increasing the levels of the neurotransmitter GABA in the brain. This can help to reduce the amount of activity in the brain during REM sleep, which can in turn reduce the occurrence and severity of episodes.
Melatonin is another medication that may be used to treat REM Sleep Behavior Disorder. It is a hormone that is naturally produced by the body, and helps to regulate our sleep-wake cycles. Melatonin supplements are often used to help people who have difficulty falling or staying asleep, and may also be helpful for managing REM Sleep Behavior Disorder symptoms. It can help to regulate circadian rhythms and improve overall sleep quality.
Antidepressants may also be used to treat REM Sleep Behavior Disorder, particularly if the underlying cause is depression or another mental health disorder. These medications can help to regulate neurotransmitters in the brain, which can improve mood, reduce anxiety, and decrease the frequency or intensity of REM sleep episodes.
It is important to note that medication should only be used under the guidance of a healthcare provider. There can be side effects, risks, and interactions with other medications to consider, and not all medications will be appropriate or effective for every individual with REM Sleep Behavior Disorder. In some cases, a combination of medications may be necessary to achieve the best results.
2. Lifestyle Changes
When it comes to treating REM Sleep Behavior Disorder (RBD), lifestyle changes play a crucial role in managing the symptoms. Here are some lifestyle changes that can be implemented:
| Lifestyle Changes | Explanation |
|---|---|
| 1. Regular Exercise | Engage in physical activity regularly to reduce stress, anxiety and depression – common risk factors for RBD. Exercise also promotes better sleep quality. |
| 2. Relaxation Techniques | Practice relaxation techniques like deep breathing, meditation and yoga to reduce stress and improve sleep quality. |
| 3. Establish Regular Sleep Patterns | Go to bed and wake up at the same time every day to maintain a healthy sleep pattern. This can help regulate sleep cycles and reduce the occurrence of RBD episodes. |
| 4. Create a Sleep-conducive Environment | Ensure that the bedroom is comfortable, quiet and cool. Use comfortable bedding and sleepwear to promote good sleep hygiene. |
| 5. Avoid Stimulants | Avoid caffeine, nicotine and alcohol close to bedtime as these can interfere with sleep quality and increase the likelihood of RBD episodes. |
It’s important to remember that not all lifestyle changes work for everyone. it is best to consult with a healthcare provider before making any drastic changes to one’s routine.
Complications of REM Sleep Behavior Disorder
REM Sleep Behavior Disorder can lead to a variety of complications that can negatively impact an individual’s quality of life. Sleep disturbances are one of the most common complications of this disorder because it can cause individuals to have trouble falling or staying asleep. The physical injuries that can occur during episodes of REM sleep, such as falling out of bed or hitting a wall, can also be a serious complication. Additionally, REM Sleep Behavior Disorder has been associated with an increased risk of developing neurodegenerative diseases such as Parkinson’s disease and other forms of dementia.
The behavior observed during these episodes can be harmful to the individual’s relationships, as they may lash out or harm their partner during an episode. This can lead to feelings of guilt and shame, as well as problems in the relationship. Another possible complication is the impact on the individual’s mental health, as the lack of restful sleep can lead to increased stress, anxiety, and depression.
REM Sleep Behavior Disorder can also have financial implications due to medical costs associated with the diagnosis and treatment of the disorder. This can include doctor visits, medications, and even hospital stays if injuries occur during an episode. Individuals with this disorder may experience occupational difficulties due to the impact that their symptoms have on their ability to perform their job duties effectively.
REM Sleep Behavior Disorder can lead to a range of complications that should not be taken lightly. Anyone experiencing symptoms of the disorder should seek medical attention to receive an accurate diagnosis and develop an appropriate treatment plan in order to minimize the risk of experiencing these negative outcomes.
Prevention of REM Sleep Behavior Disorder
It can be difficult to completely prevent REM Sleep Behavior Disorder (RBD), as it is often a result of underlying neurodegenerative or genetic factors. However, there are some steps that can be taken to potentially reduce an individual’s risk or delay the onset of symptoms.
Maintain a Consistent Sleep Schedule: Establishing a regular sleep schedule can promote healthy sleep habits and potentially decrease the likelihood of experiencing RBD symptoms. This involves going to bed and waking up at the same time each day, even on weekends.
Avoid Alcohol and Sedatives: Alcohol and sedatives have been linked to an increased risk of RBD. Limiting or avoiding the consumption of these substances may decrease the likelihood of developing symptoms.
Treat Underlying Sleep Disorders and Mental Health Conditions: Addressing underlying sleep disorders or mental health conditions, such as anxiety or depression, may reduce the risk of developing RBD symptoms.
Stay Active and Maintain a Healthy Lifestyle: Engaging in regular physical activity and maintaining a healthy diet may decrease the risk of developing RBD. It is important to speak with a healthcare professional before starting any new exercise or diet regimen.
While it may not be possible to completely prevent RBD, there are steps that can be taken to potentially reduce an individual’s risk. Maintaining healthy sleep habits, avoiding alcohol and sedatives, treating underlying conditions, and staying active may all play a role in decreasing the likelihood of developing RBD.
Conclusion
In conclusion, REM Sleep Behavior Disorder is a complex and intriguing condition that warrants further study and understanding. The causes of this disorder vary widely, ranging from neurological conditions to genetics to medications and substances, and certain risk factors can predispose individuals to developing the disorder.
Symptoms of the disorder can be severe and disruptive to daily life, but with proper diagnosis and treatment, individuals can manage or even control their symptoms, leading to improved overall quality of life.
While medications and lifestyle changes can help reduce symptoms and complications, it’s important to note that REM Sleep Behavior Disorder can potentially lead to serious complications, such as injury or even death.
Therefore, preventing the disorder through healthy sleep habits and avoiding risk factors when possible, such as certain medications or substances, is crucial for maintaining overall health and well-being.
As with many medical conditions, early diagnosis and treatment can greatly improve outcomes, making it essential for individuals experiencing symptoms to seek medical attention as soon as possible.
Overall, the study of REM Sleep Behavior Disorder serves as a reminder of the profound complexity of the human brain and the intricacies of the sleep-wake cycle. Continued research and understanding of this disorder can lead to improved treatment options and quality of life for those affected.
Frequently Asked Questions
1. Can REM Sleep Behavior Disorder be cured?
While there is no cure for REM Sleep Behavior Disorder, it can be managed with medications and lifestyle changes.
2. Is REM Sleep Behavior Disorder the same as sleepwalking?
No, REM Sleep Behavior Disorder is different from sleepwalking. Those with REM Sleep Behavior Disorder act out their dreams, while sleepwalking involves walking around without being fully awake.
3. Can medications cause REM Sleep Behavior Disorder?
Yes, certain medications like antidepressants, antipsychotics, and medications used for Parkinson’s disease can cause REM Sleep Behavior Disorder.
4. Can alcohol consumption lead to REM Sleep Behavior Disorder?
Alcohol consumption can increase the risk of REM Sleep Behavior Disorder, particularly if consumed close to bedtime.
5. How is REM Sleep Behavior Disorder diagnosed?
REM Sleep Behavior Disorder is diagnosed through a combination of a physical exam, sleep history, and a polysomnogram (sleep study).
6. Is REM Sleep Behavior Disorder hereditary?
There is evidence that genetics can play a role in the development of REM Sleep Behavior Disorder.
7. Can REM Sleep Behavior Disorder cause injury?
Yes, those with REM Sleep Behavior Disorder can injure themselves or their partner while acting out their dreams.
8. Are there any natural remedies for treating REM Sleep Behavior Disorder?
While there is no specific natural remedy for REM Sleep Behavior Disorder, generally improving sleep hygiene can help. This includes maintaining a consistent sleep schedule, avoiding stimulants before bed, and creating a relaxing bedtime routine.
9. Can REM Sleep Behavior Disorder affect cognitive function?
There is some evidence to suggest that REM Sleep Behavior Disorder may be associated with cognitive decline and an increased risk of developing neurodegenerative diseases like Parkinson’s disease and dementia.
10. Is it possible to prevent REM Sleep Behavior Disorder?
While there is no surefire way to prevent REM Sleep Behavior Disorder, individuals can reduce their risk by maintaining a healthy sleep routine, avoiding alcohol close to bedtime, and talking to their doctor if they are taking medications that may increase the risk of the disorder.