Sleep is a crucial element for the overall well-being of an individual. It offers a chance for the body to repair, reorganize, and rejuvenate itself. However, some individuals experience difficulty in maintaining a regular sleep-wake cycle due to a sleep disorder called narcolepsy. Narcolepsy is a neurological disorder that affects the ability to regulate sleep-wake cycles. It is often characterized by excessive daytime sleepiness and sudden sleep attacks. While the underlying causes of narcolepsy are yet to be fully understood, current research has provided insights into its science, types, and symptoms. This article aims to explore narcolepsy in detail, including its impact on sleep and dreaming and the available treatment options.
The Science behind Narcolepsy
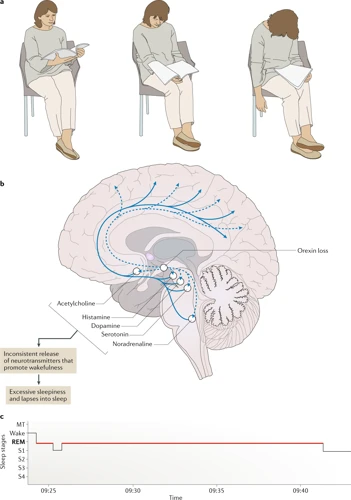
Understanding the intricate workings of the brain is no easy feat, but it is crucial in comprehending the science behind conditions like narcolepsy. Narcolepsy is a neurological disorder that impacts the brain’s ability to regulate sleep-wake cycles and can cause excessive daytime sleepiness, sudden muscle weakness, and even hallucinations. The complex mechanisms that underlie this disorder involve a variety of neurotransmitters and receptors in the brain, such as those involved in regulating arousal, mood, and motor function. In this section of the article, we will delve deeper into the intricate science behind narcolepsy and explore what makes it such a unique and challenging condition to manage.
The Different Types of Narcolepsy
Narcolepsy is classified into several types based on the symptoms experienced by an individual. Here are the different types of Narcolepsy:
- Narcolepsy type 1: This type of narcolepsy is severe and more common. People with narcolepsy type 1 tend to have episodes of cataplexy, which is a sudden loss of muscle tone that can cause weakness or complete collapse. It is often triggered by strong emotions such as laughter or anger. Additionally, individuals with narcolepsy type 1 experience extreme daytime sleepiness, hypnagogic hallucinations, and sleep paralysis.
- Narcolepsy type 2: This type of narcolepsy is less severe than type 1 but still causes significant disruption to sleep and daytime functioning. People with narcolepsy type 2 experience extreme daytime sleepiness and may also have episodes of sleep paralysis, hypnagogic hallucinations, and automatic behaviors. However, they do not suffer from cataplexy.
- Pseudo-narcolepsy: This type of narcolepsy is caused by other underlying medical conditions such as sleep apnea, depression, or anxiety disorders. The symptoms are similar to those of narcolepsy but are not caused by a dysfunction in the brain’s sleep-wake cycle.
It is important to note that only a sleep specialist can diagnose narcolepsy accurately. Identifying the type of narcolepsy is crucial in developing an appropriate treatment plan.
The Symptoms of Narcolepsy
Narcolepsy is a chronic sleep disorder that affects approximately 1 in every 2,000 people. It can have a significant impact on a person’s daily life, causing them to feel excessively sleepy during the day and experiencing sudden urges to sleep. Here are some of the most common symptoms of narcolepsy:
- Excessive daytime sleepiness: People with narcolepsy may feel drowsy and have an irresistible urge to sleep multiple times throughout the day, even if they have had a full night’s rest. This can make it difficult to concentrate and stay alert during work or school.
- Sudden loss of muscle control (cataplexy): Cataplexy is a sudden loss of muscle tone or control that can be brought on by strong emotions such as laughter, anger, or surprise. During a cataplexy episode, the affected person may have difficulty moving or speaking.
- Hallucinations: Narcolepsy can cause vivid and often frightening hallucinations, even when a person is fully awake. These hallucinations may be visual, auditory, or tactile in nature, and can often lead to confusion or distress.
- Sleep paralysis: Sleep paralysis is a temporary inability to move or speak that occurs upon waking up or falling asleep. During an episode of sleep paralysis, a person may be fully aware of their surroundings but unable to move their body or speak.
- Fragmented nighttime sleep: Narcolepsy can cause nighttime sleep disruptions, such as frequent awakenings or difficulty staying asleep throughout the night.
If you are experiencing any of these symptoms, it is important to speak with a healthcare professional for a proper diagnosis and treatment plan.
Sleep and Narcolepsy
As we delve deeper into the world of narcolepsy, it becomes apparent that this disorder not only affects wakefulness but also has a significant impact on sleep. Understanding the relationship between sleep and narcolepsy is crucial in comprehending the complexities of this condition. Let’s take a closer look at how narcolepsy affects sleep and the various stages of sleep affected by this condition.
The Stages of Sleep
During sleep, the brain goes through different stages of activity, each with its own unique characteristics and functions. Understanding these stages is important in understanding how narcolepsy affects sleep. There are typically four stages of non-REM (NREM) sleep and one stage of REM sleep.
| Stage | Description | Brain Waves |
|---|---|---|
| Stage N1 | The transition between wakefulness and sleep. This stage usually lasts only a few minutes. | Theta Waves |
| Stage N2 | The period of light sleep. It accounts for the majority of our sleep cycle. | Sleep Spindles K-Complexes |
| Stage N3 | The period of deep sleep. It is often referred to as slow-wave sleep (SWS). | Delta Waves |
| Stage N4 | The deepest stage of sleep. It is difficult to wake up from this stage. | Delta Waves |
| REM Sleep | The stage where dreaming occurs. The body is paralyzed, and brain activity resembles that of a person who is awake. | Low-Amplitude Mixed Frequency Waves |
During a typical sleep cycle, a person goes through all the stages of sleep multiple times, with more time spent in the lighter stages of sleep at the beginning of the night and more time spent in the deeper stages of sleep later in the night. Narcolepsy can have a significant impact on the amount of time spent in each stage of sleep, particularly on REM sleep.
How Narcolepsy Affects Your Sleep
Narcolepsy can have a significant impact on sleep quality and quantity. Let’s take a look at how narcolepsy affects sleep in the table below:
| Average Sleeper | Narcoleptic Sleeper | |
|---|---|---|
| Time to Fall Asleep | 10-20 minutes | Virtually immediate (during the day) |
| Sleep Onset REM Period (SOREMP) | Does not occur | Occurs within 15 minutes of falling asleep during the day |
| Number of Nighttime Awakenings | 1-2 | More frequent due to disrupted sleep-wake cycle |
| Sleep Efficiency | Around 90% | Lower due to interrupted sleep |
| Total Sleep Time | Average of 7-9 hours | May be as little as 2-3 hours, with daytime naps making up the rest of the necessary sleep |
As we can see, narcolepsy can lead to a number of disruptions in typical sleep patterns. It may be difficult to fall asleep at night, but during the day, narcoleptic individuals may experience sudden sleep attacks, falling asleep immediately and without warning. These daytime sleep attacks may be accompanied by a phenomenon known as Sleep Onset REM Period (SOREMP), which involves entering directly into REM sleep upon falling asleep. This can lead to vivid dreaming and other disruptions in daytime activities.
Nighttime sleep may be interrupted, leading to more frequent awakenings and lower sleep efficiency overall. Total sleep time may also be reduced, with individuals sometimes only getting a few hours of nighttime sleep and making up the rest of their necessary sleep through daytime naps. All of these disruptions can lead to excessive daytime sleepiness and decreased overall quality of life.
Dreaming and Narcolepsy

As we explore the intricacies of narcolepsy, it’s important to delve into the relationship between dreaming and this sleep disorder. Dreaming is an essential part of the sleep cycle, and it plays a critical role in our overall health and well-being. For individuals with narcolepsy, the relationship between dreaming and sleep becomes even more complex. Let’s take a closer look at how narcolepsy can affect dreaming and what implications this can have for those who live with this condition.
The Relationship between Dreams and Sleep
During sleep, human beings experience a variety of dreams. Dreams are a natural part of the sleep cycle and occur during the REM (Rapid Eye Movement) stage of sleep. During this stage, the brain is highly active, and it is thought that the vivid, sensory experiences of dreaming are a result of this increased activity.
Dreams are often characterized by vivid and sometimes bizarre imagery, as well as strong emotions such as fear, joy, and sadness. They may tell a story or consist of fragmented, disconnected images. While the exact function of dreaming is not fully understood, it is believed that dreams serve a variety of purposes, from processing emotions to consolidating memories.
One of the hallmarks of narcolepsy is a disruption in the normal sleep cycle, including the REM stage of sleep. As a result, people with narcolepsy may experience disruptions in their dreams as well. Some individuals with narcolepsy report experiencing vivid, intense dreams, while others may have difficulty recalling their dreams or may not dream at all.
The relationship between dreaming and sleep is complex and still not fully understood. However, it is clear that disruptions in the normal sleep cycle, such as those experienced by people with narcolepsy, can have an impact on dreaming. By better understanding the relationship between sleep and dreaming, researchers may be able to develop new treatments for narcolepsy and other sleep disorders.
The Impact of Narcolepsy on Dreaming
Dreams serve as a window to our unconscious mind, but for people with narcolepsy, the boundary between sleep and wakefulness is blurred, leading to some unique impacts on their dreaming. Here are some ways in which narcolepsy impacts the dreaming process:
- Dreams during daytime naps: One hallmark of narcolepsy is excessive daytime sleepiness, and those with the condition may take frequent daytime naps. During these naps, people with narcolepsy can enter into dreaming sleep quickly, and these dreams can be more vivid than those experienced during nighttime sleep. This is because daytime sleep tends to include more REM (rapid eye movement) sleep, which is the stage of sleep during which most dreaming occurs.
- Fragmented dreams: Due to the disrupted nature of narcolepsy, the sleep cycle may be interrupted, leading to fragmented and disjointed dreams. This can make it difficult for people with narcolepsy to remember their dreams, and they may instead experience dream-like hallucinations during wakefulness.
- Vivid, intense dreams: People with narcolepsy often experience very vivid and often intense dreams, which can sometimes be disturbing or overwhelming. This may be due to the fact that narcolepsy disrupts the timing and depth of sleep, leading to more intense dream experiences.
- REM intrusion: In some cases, people with narcolepsy may experience a phenomenon known as REM intrusion, in which they have vivid dream-like episodes during wakefulness. This can be disorienting and can interfere with daily activities.
Understanding the impact of narcolepsy on dreaming can help individuals with the condition better manage their symptoms and get the treatment they need to improve their overall quality of life.
Treatment for Narcolepsy
After being diagnosed with narcolepsy, finding an effective treatment plan is crucial for managing the condition. Treatment options for narcolepsy range from medication to lifestyle changes. However, the best course of action often involves a combination of both. In this section, we will explore the various options available for treating narcolepsy, including the role of medication and lifestyle changes in improving sleep and managing symptoms. It’s important to note that there is no cure for narcolepsy, but with the right treatment plan, those with the condition can live full and productive lives.
The Role of Medication in Managing Narcolepsy
When it comes to managing narcolepsy, medication can be a crucial component in helping individuals cope with their symptoms. There are several types of medication that can be prescribed, each with its own benefits and potential side effects. Here is a breakdown of some of the most common medication options:
| Medication | How it Works | Potential Side Effects |
|---|---|---|
| Stimulants | These medications help increase alertness and reduce daytime sleepiness by stimulating the central nervous system. | Insomnia, jitteriness, anxiety, increased heart rate and blood pressure. |
| Modafinil | This drug helps promote wakefulness and reduce daytime sleepiness by altering the levels of certain neurotransmitters in the brain. | Headache, nausea, dizziness, insomnia, anxiety. |
| Sodium Oxybate | This medication is taken at night and helps improve the quality of nighttime sleep. It can also reduce the symptoms of cataplexy. | Nausea, dizziness, headache, bedwetting, worsening of sleep apnea. |
It is important to note that medication is not a one-size-fits-all solution and each individual may have different responses and reactions to different medications. It is important to work closely with a healthcare provider to find the medication and dosage that works best for each individual.
In addition to medication, lifestyle changes can also be helpful in managing narcolepsy symptoms. This can include maintaining a regular sleep schedule, avoiding caffeine and alcohol, and incorporating regular exercise into a daily routine. By taking a comprehensive approach to managing narcolepsy, individuals can improve their overall quality of life and reduce the impact that this condition has on their daily activities.
Lifestyle Changes to Improve Sleep and Manage Narcolepsy
Making lifestyle changes can significantly improve the symptoms of narcolepsy and help manage the condition. Here are some lifestyle changes you can incorporate into your daily routine:
- Stick to a sleep schedule: Try to go to bed and wake up at the same time every day, including weekends. Consistency can help regulate your body’s natural sleep-wake cycle.
- Take short naps: Plan to take short, scheduled naps throughout the day to help manage excessive daytime sleepiness. Keep naps to 20-30 minutes to avoid interfering with nighttime sleep.
- Avoid caffeine and alcohol: Stimulants like caffeine can interfere with sleep, and alcohol can disrupt the quality of your sleep. Avoid consuming these substances close to bedtime.
- Exercise regularly: Regular physical activity can help improve the quality of your sleep and reduce daytime sleepiness. Aim for at least 30 minutes of moderate exercise most days of the week.
- Create a relaxing bedtime routine: Engage in calming activities before bed to help prepare your body for sleep. This might include taking a warm bath or shower, reading a book, or practicing relaxation techniques such as yoga or meditation.
- Evaluate your sleep environment: Make sure your bedroom is quiet, dark, and cool. Consider investing in a comfortable mattress and pillows to improve your sleep quality.
- Manage stress: Stress can interfere with sleep and exacerbate narcolepsy symptoms. Find healthy ways to manage stress, such as exercise, meditation, or therapy.
Remember, these changes cannot cure narcolepsy, but they can help alleviate symptoms and improve sleep quality. Over time, incorporating these habits into your daily routine can become a natural part of your lifestyle, contributing to your overall health and wellbeing.
Conclusion
After exploring narcolepsy and its effects on sleep and dreaming, it is clear that it can significantly impact a person’s quality of life. It is an understudied and often misunderstood disorder, but with awareness and proper diagnosis, individuals with narcolepsy can manage their symptoms effectively.
The Importance of Seeking Medical Attention: If you or a loved one suspect that you may have symptoms of narcolepsy, it is important to seek medical attention. Narcolepsy is a chronic condition that requires ongoing management. Proper diagnosis and treatment can help individuals lead fulfilling lives despite the disorder.
Treating Narcolepsy: There is no cure for narcolepsy, but medications, lifestyle changes, and behavioral therapies can help manage symptoms. Stimulants such as methylphenidate and modafinil can improve alertness and reduce the frequency of daytime sleep attacks. Antidepressants and sodium oxybate are also used in the treatment of narcolepsy.
Lifestyle Changes: Making small lifestyle changes can also make a big difference in managing narcolepsy. Practicing good sleep hygiene, such as establishing a consistent sleep schedule and avoiding caffeine and alcohol, can help regulate sleep. Exercise, a healthy diet, and stress reduction techniques such as meditation and relaxation exercises can also help manage symptoms.
Support: Support from family, friends, and support groups can also be invaluable in managing narcolepsy. It can also help to find a job or career that is flexible and accommodating to the disorder.
In conclusion, narcolepsy is a complex neurological disorder that impacts an individual’s sleep and daytime functioning. However, with proper diagnosis, treatment, and lifestyle changes, individuals with narcolepsy can lead fulfilling and productive lives. Seeking medical attention, managing symptoms with medication and lifestyle changes, and finding support are all key to managing this disorder.
Frequently Asked Questions
What causes narcolepsy?
The exact cause of narcolepsy is unknown, but it is thought to be a combination of genetic and environmental factors.
Is narcolepsy a rare condition?
Yes, narcolepsy is considered a rare condition that affects approximately 1 in 2,000 people.
Can narcolepsy be cured?
There is currently no cure for narcolepsy, but symptoms can be managed with medication and lifestyle changes.
What medications are used to treat narcolepsy?
Stimulants, such as modafinil and armodafinil, are commonly used to treat the excessive daytime sleepiness associated with narcolepsy. Sodium oxybate is also used to treat cataplexy and improve nighttime sleep.
What lifestyle changes can help manage narcolepsy?
Establishing a regular sleep schedule, avoiding caffeine and alcohol, and taking short naps during the day can all help manage symptoms of narcolepsy.
Can narcolepsy affect your ability to drive?
Yes, the excessive daytime sleepiness and sudden onset of sleep associated with narcolepsy can make it dangerous to drive. People with narcolepsy should inform their doctor and take necessary precautions when driving.
Do all people with narcolepsy experience cataplexy?
No, not all people with narcolepsy experience cataplexy. It is estimated that approximately 70% of people with narcolepsy type 1 will experience cataplexy.
Can narcolepsy be diagnosed through a sleep study?
Yes, a sleep study called a polysomnogram with Multiple Sleep Latency Test (MSLT) can be used to diagnose narcolepsy.
Is there a difference between narcolepsy type 1 and narcolepsy type 2?
Yes, narcolepsy type 1 is characterized by excessive daytime sleepiness and cataplexy, while narcolepsy type 2 is characterized by excessive daytime sleepiness without cataplexy.
Can stress make narcolepsy symptoms worse?
Yes, stress can trigger or worsen symptoms of narcolepsy, such as excessive daytime sleepiness and cataplexy.