It’s not uncommon to feel exhausted during the day, but what if it’s more than just a lack of sleep? Some individuals experience excessive daytime sleepiness, sudden sleep attacks, and even cataplexy, which can be signs of a sleep disorder called narcolepsy. While this condition affects only a small number of people, it can have a significant impact on their quality of life. In this article, we’ll explore what narcolepsy is, its causes and symptoms, as well as the diagnostic process and treatment options available. So, let’s delve into this perplexing condition and learn more about how it’s diagnosed and managed.
What Is Narcolepsy?
Narcolepsy is a perplexing neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. Individuals with narcolepsy often experience overwhelming daytime sleepiness and uncontrollable episodes of falling asleep during the day. These episodes can occur at any time and can be triggered by emotional or physical stimuli. Narcolepsy can have a significant impact on a person’s quality of life as it can interfere with their ability to perform daily activities, including work or social interactions. Let’s explore the symptoms and causes of narcolepsy in more detail.
Symptoms
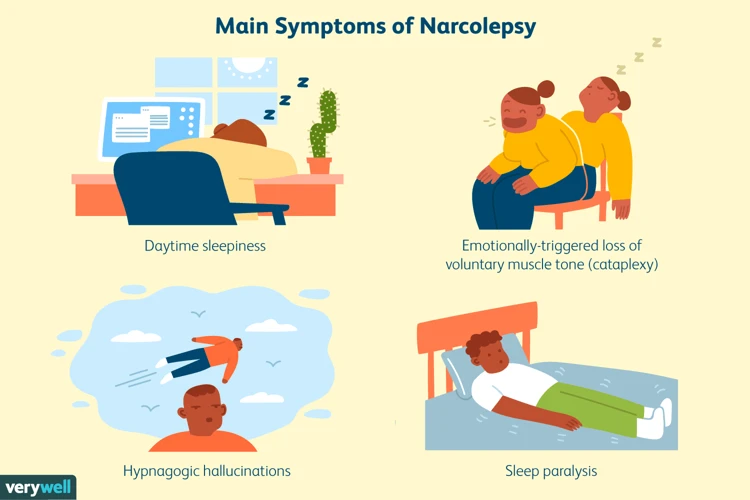
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles, resulting in excessive daytime sleepiness and other symptoms. Below are some common symptoms that a person with narcolepsy may experience:
| SYMPTOM | DESCRIPTION |
|---|---|
| Excessive Daytime Sleepiness (EDS) | Feeling excessively sleepy during the day, despite getting enough sleep at night. |
| Cataplexy | A sudden loss of muscle tone, often triggered by intense emotions. |
| Sleep Paralysis | A temporary inability to move or speak when waking up or falling asleep. |
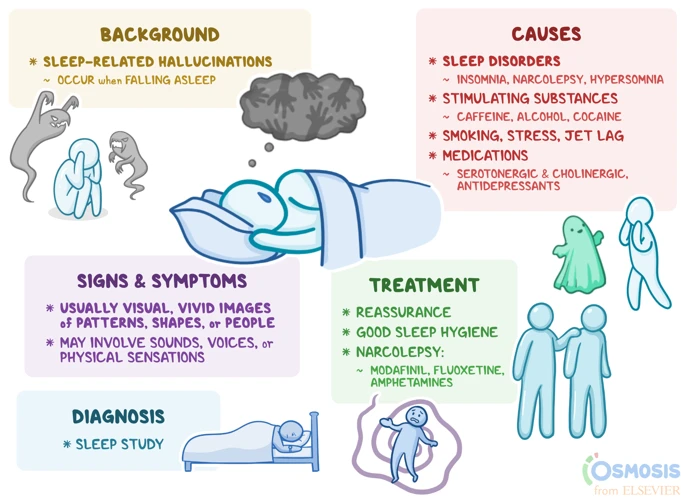
| Hypnagogic Hallucinations | Vivid and often frightening hallucinations that occur when falling asleep. |
| Fragmented Nighttime Sleep | Difficulty staying asleep through the night, often waking up frequently. |
It is important to note that not all individuals with narcolepsy will experience all of these symptoms. In fact, some people may only have daytime sleepiness without any other noticeable symptoms. It is also worth highlighting that these symptoms can often be mistaken for other sleep disorders or medical conditions, which is why a proper diagnosis is crucial.
Causes
Narcolepsy is a neurological disorder whose causes are not fully understood. It’s believed that a combination of genetic and environmental factors may contribute to its development. Here are some of the known potential causes of narcolepsy:
- Genetics: Narcolepsy tends to run in families. Research has found that certain genes may increase a person’s susceptibility to the disorder.
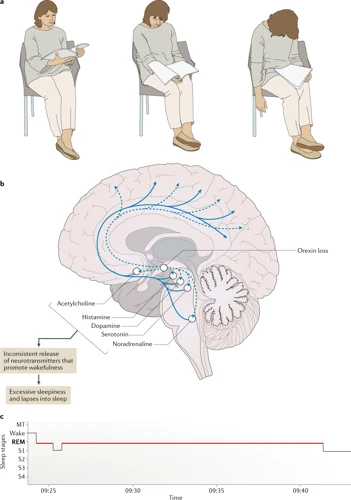
- Hypocretin deficiency: The main cause of narcolepsy with cataplexy is the lack of hypocretin, a neurotransmitter that plays a role in regulating wakefulness and sleep.
- Autoimmune response: Some researchers believe that narcolepsy may be an autoimmune disorder, where the immune system mistakenly attacks and destroys the hypocretin-producing cells in the brain.
- Brain injury: In some cases, a head injury or trauma to the brain has been linked to the onset of narcolepsy.
- Infections: Certain infections, such as streptococcal infections, have been associated with narcolepsy. It’s thought that the infection may trigger an autoimmune response.
- Chemical imbalance in the brain: Imbalances in the levels of neurotransmitters that regulate sleep and wakefulness, such as dopamine and norepinephrine, may also play a role in narcolepsy.
It’s important to note that while these factors may increase the likelihood of developing narcolepsy, not everyone with these risk factors will develop the disorder.
Diagnostic Process
When struggling with daytime sleepiness, chronic fatigue, and sudden loss of muscle control, it is important to seek medical attention to determine the cause of these symptoms. One possible explanation for these symptoms is narcolepsy, a neurological disorder that affects a person’s ability to regulate their sleep-wake cycle. The diagnostic process for narcolepsy involves a series of evaluations, medical history and physical exams, as well as sleep studies and diagnostic tests. Let’s take a closer look at how narcolepsy is diagnosed.
Evaluation of Symptoms
Evaluation of Symptoms
The first step in the diagnostic process for narcolepsy is often an evaluation of the patient’s symptoms. This typically involves a discussion between the patient and their doctor about the specific symptoms they are experiencing. The doctor will ask questions to determine the type and severity of symptoms the patient is experiencing.
Often, patients with narcolepsy experience excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), sleep paralysis, and/or hallucinations. These symptoms can interfere with daily life and can be dangerous if they occur during activities such as driving or operating machinery.
To evaluate symptoms, doctors may use a standardized questionnaire, such as the Epworth Sleepiness Scale, which asks the patient to rate their level of sleepiness during certain activities. The doctor may also assess the patient’s ability to stay awake during the day by using a sleep latency test or a maintenance of wakefulness test.
In addition to these symptoms, patients with narcolepsy may also experience disturbed nighttime sleep, insomnia, and/or restless leg syndrome. It is important for the doctor to ask about all of these symptoms to get a full picture of the patient’s sleep patterns and difficulties.
The table below summarizes the common symptoms of narcolepsy and how they may affect an individual:
| Symptom | Description | Effects |
|---|---|---|
| Excessive daytime sleepiness (EDS) | Ongoing feeling of sleepiness and a lack of energy during the day | Difficulty staying awake during normal activities, increased risk of accidents and mistakes |
| Cataplexy | Sudden loss of muscle tone and control in response to strong emotions | May lead to falls or injury, can cause social anxiety and embarrassment |
| Sleep paralysis | Temporary inability to move or speak when waking up or falling asleep | May cause anxiety or fear, can transform into hallucinations |
| Hallucinations | Seeing, hearing or feeling things that are not real, often during sleep or waking up | Confusion and fear, can lead to anxiety and depression |
By evaluating the patient’s symptoms, doctors can gain an understanding of whether narcolepsy may be the cause of their sleep disturbances. This information can help to guide further diagnostic testing and treatment decisions.
Medical History and Physical Exam
During the diagnostic process for narcolepsy, a medical history and physical examination are often conducted to gather more information about the patient’s symptoms and overall health. This step in the process is crucial towards helping doctors form a complete diagnosis and creating an effective treatment plan.
Medical History
The medical history portion of the process involves the medical professional asking questions about the patient’s overall health, any medications they may be taking, and their sleep patterns. The doctor will also ask about any past or present medical conditions that may be contributing to the patient’s symptoms.
To keep track of this information, the doctor may use an html table to organize the data. This table can include columns for the patient’s medical history, medications, and any other relevant information that may help the doctor form a more complete diagnosis.
Physical Exam
The physical exam involves a health care provider checking the patient’s vital signs, such as blood pressure and heart rate, as well as looking for any physical symptoms of narcolepsy or other conditions that may be contributing to the patient’s symptoms.
During a physical exam, a medical professional may also assess the patient’s muscle tone and reflexes, as these can be affected by narcolepsy. These results may be recorded in another html table as well to keep track of the data.
The medical history and physical exam are important steps in the process of diagnosing narcolepsy. By gathering information about the patient’s health history and checking for any physical symptoms, doctors can form a more accurate diagnosis and create a treatment plan that will best address their patient’s symptoms.
Sleep Studies and Diagnostic Tests
To confirm a narcolepsy diagnosis, sleep studies and diagnostic tests are normally conducted. These tests may include the following:
- Nocturnal polysomnography: This sleep study is conducted overnight in a sleep lab. It monitors the patient’s brain waves, heart rate, breathing, and limb movements while they sleep.
- Multiple sleep latency test: This test is conducted during the day, and involves the patient taking a series of naps. It is used to measure how long it takes the patient to fall asleep, and whether they enter rapid eye movement (REM) sleep quickly.
- Human leukocyte antigen (HLA) genetic blood test: This test is used to identify whether the patient has a specific genetic marker that is associated with narcolepsy.
- Cerebrospinal fluid analysis: A sample of cerebrospinal fluid may be taken from the patient to check whether levels of hypocretin – a chemical that regulates wakefulness – are lower than normal. This test is typically done with a lumbar puncture, which involves inserting a needle into the lower back and extracting a small amount of fluid.
It is important to note that these tests are not always necessary to make a narcolepsy diagnosis. The symptoms that a patient presents with, as well as their medical history and physical exam, may provide enough evidence to confirm a diagnosis. Nevertheless, sleep studies and diagnostic tests can help rule out other conditions that may have similar symptoms, and are therefore an important part of the diagnostic process.
Treatment Options
As with any medical condition, effective treatment for narcolepsy is crucial for managing its symptoms and improving the quality of life. There are several approaches to treating narcolepsy, including medications, lifestyle changes, and supportive therapies. While each person with narcolepsy may require a different treatment plan, finding the right combination of interventions can help them lead a more fulfilling and productive life. Let’s delve deeper into the various options available for treating narcolepsy.
Medications
One of the primary treatment options for narcolepsy is the use of medications. These drugs can help to manage the symptoms and improve the quality of life for those with this disorder. Let’s take a closer look at some of the medications that may be prescribed to treat narcolepsy:
| Medication | How it Works | Possible Side Effects |
|---|---|---|
| Stimulants | Stimulants work by increasing levels of alertness and reducing the tendency to fall asleep. They can help with excessive daytime sleepiness. | Insomnia, anxiety, irritability, increased blood pressure, rapid heartbeat. |
| Modafinil (Provigil) | Modafinil is a wakefulness-promoting agent that works by altering the levels of neurotransmitters in the brain. It can help to reduce excessive daytime sleepiness and improve cognitive performance. | Headache, nausea, dizziness, back pain, nervousness. |
| Sodium Oxybate (Xyrem) | Sodium oxybate is a central nervous system depressant that can help to regulate sleep-wake cycles. It can improve overall sleep quality and reduce the frequency of nighttime awakenings, as well as improve symptoms of cataplexy. | Nausea, dizziness, confusion, sleepwalking, respiratory depression. |
It’s important to note that these medications should be prescribed and monitored by a healthcare professional, as they can have potential side effects and may interact with other medications or medical conditions. In addition to medications, lifestyle changes and supportive therapies can also be effective in managing narcolepsy symptoms.
Lifestyle Changes
Making positive lifestyle changes can significantly improve narcolepsy symptoms and increase overall quality of life. Here are some lifestyle modifications that can help manage narcolepsy:
- Establish a consistent sleep schedule: Going to bed and waking up at the same time every day can help regulate the body’s sleep-wake cycle and improve symptoms.
- Avoid caffeine and alcohol: These substances can disrupt sleep and worsen narcolepsy symptoms.
- Take short naps: Planned, short naps during the day can help reduce daytime sleepiness.
- Exercise regularly: Regular exercise can boost energy levels and improve mood. However, it’s important to avoid exercising close to bedtime.
- Avoid large meals before bedtime: Eating a heavy meal before bedtime can interfere with sleep quality.
- Eliminate distractions: Minimizing distractions in the sleep environment, such as noise and light, can improve sleep quality.
- Seek emotional and social support: Living with narcolepsy can be challenging. It is important to seek support from friends, family, and support groups to manage the emotional toll of the condition.
Making these lifestyle changes, in combination with medical treatment, can help manage narcolepsy symptoms and improve overall quality of life.
Supportive Therapies
Supportive therapies are an essential part of narcolepsy treatment since they help improve the quality of life for people with narcolepsy. These therapies aim to eliminate or alleviate the symptoms of narcolepsy and help people with this disorder manage their symptoms better.
One example of a supportive therapy for narcolepsy is occupational therapy. This therapy helps people with narcolepsy improve their ability to perform daily activities by providing them with tools and techniques to manage their symptoms. Occupational therapists can help people with narcolepsy learn how to plan their day and break down complex tasks into smaller and manageable steps that can reduce fatigue and improve productivity.
Another supportive therapy for narcolepsy is cognitive-behavioral therapy (CBT). CBT is a type of talk therapy that can help people with narcolepsy manage their symptoms by helping them identify negative thoughts and behaviors that can worsen their symptoms. CBT can also help people with narcolepsy develop coping strategies to manage their symptoms and improve their overall quality of life.
People with narcolepsy can also benefit from sleep hygiene education. Sleep hygiene education involves learning good sleep habits that can improve the quality of sleep and help people with narcolepsy manage their symptoms better. For example, maintaining a regular sleep schedule, avoiding caffeine and alcohol, and ensuring a comfortable sleeping environment can all help improve the quality of sleep for individuals with narcolepsy.
Support groups can also be helpful for individuals with narcolepsy. Joining a support group allows individuals with narcolepsy to connect with others who understand their experiences and struggles. Support groups can provide valuable emotional support, practical advice, and tips on how to manage the symptoms of narcolepsy.
The following table summarizes the different supportive therapies for narcolepsy:
| Supportive Therapies for Narcolepsy |
|---|
| Occupational Therapy |
| Cognitive-Behavioral Therapy (CBT) |
| Sleep Hygiene Education |
| Support Groups |
Supportive therapies play an important role in the overall management of narcolepsy. These therapies can help individuals with narcolepsy manage their symptoms, improve their quality of life, and connect with others who understand their experiences. Along with medication and lifestyle changes, supportive therapies can help individuals with narcolepsy take control of their lives and achieve their goals.
Conclusion
In conclusion, narcolepsy is a neurological disorder that can significantly affect a person’s daily life. Its symptoms can range from excessive daytime sleepiness and sudden muscle weakness to hallucinations and sleep paralysis.
Diagnosis of narcolepsy can be challenging, as its symptoms can be easily attributed to other conditions. However, with the correct evaluation of symptoms, medical history and physical exams, and sleep studies, it is possible to diagnose narcolepsy accurately.
Treatment options for narcolepsy typically include a combination of medications, lifestyle changes, and supportive therapies. Medications such as modafinil and sodium oxybate can help to alleviate symptoms and improve wakefulness, while lifestyle changes like regular exercise and healthy sleep habits can promote overall health and well-being.
Supportive therapies, such as counseling and support groups, can also play a significant role in helping individuals cope with the emotional and social effects of narcolepsy.
It’s essential to note that the treatment of narcolepsy is not a one-size-fits-all approach. Each individual’s treatment plan may vary based on their specific needs and circumstances. It’s crucial to work closely with a healthcare provider to develop a treatment plan that is tailored to your needs and preferences.
Overall, with proper diagnosis and management, individuals with narcolepsy can lead fulfilling and productive lives. The key is to seek medical attention if you suspect you may have narcolepsy and to work closely with your healthcare team to manage your symptoms effectively.
Frequently Asked Questions
How is narcolepsy diagnosed?
Narcolepsy is diagnosed through a combination of evaluation of symptoms, medical history, physical exam, and sleep studies or diagnostic tests.
What are the symptoms of narcolepsy?
The symptoms of narcolepsy include excessive daytime sleepiness, sudden muscle weakness, sleep paralysis, and hallucinations.
What causes narcolepsy?
The specific cause of narcolepsy is unknown, but it is believed to be a combination of genetic and environmental factors.
What is a sleep study?
A sleep study is a diagnostic test typically performed overnight in a sleep laboratory to evaluate a person’s sleep patterns, brain activity, and breathing during sleep.
What medications are used to treat narcolepsy?
Stimulants such as modafinil, armodafinil, and methylphenidate are commonly used to treat excessive daytime sleepiness in narcolepsy. Sodium oxybate is also used to improve nighttime sleep and reduce daytime sleepiness.
What lifestyle changes can help manage narcolepsy?
Establishing a regular sleep schedule, taking short naps during the day, and avoiding alcohol and caffeine can help manage narcolepsy symptoms.
Can narcolepsy be cured?
There is no cure for narcolepsy, but it can be managed through medications and lifestyle changes.
Is narcolepsy a rare condition?
Narcolepsy is considered a rare condition, affecting approximately 1 in 2,000 people.
Can narcolepsy affect a person’s quality of life?
Yes, narcolepsy can significantly affect a person’s quality of life, impacting their ability to work, drive, and engage in daily activities.
Can narcolepsy be misdiagnosed?
Yes, narcolepsy can be misdiagnosed as another sleep disorder, such as sleep apnea or restless leg syndrome, due to similar symptoms. This is why proper evaluation and testing is crucial for an accurate diagnosis.