Narcolepsy has always been shrouded in mystery, leaving both medical professionals and those living with the condition perplexed. From sudden bouts of sleep to vivid hallucinations, it’s a complex disorder that can severely impact someone’s life. But what causes this baffling condition? And how can it be treated? In this scientific exploration, we’ll delve into the world of narcolepsy, unlocking some of its biggest mysteries and exploring cutting-edge research aimed at bringing us closer to understanding and managing this enigmatic disorder.
What is Narcolepsy?
Narcolepsy is a baffling neurological disorder that affects thousands of people worldwide. It is a condition that perplexes even the most knowledgeable experts in the field of sleep medicine. Narcolepsy is often misunderstood and misdiagnosed, leaving individuals feeling frustrated, isolated, and exhausted. Understanding this debilitating condition is crucial in order to provide appropriate care and support to those who suffer from it. Let’s delve into this complex topic and uncover the mysteries of narcolepsy.
Symptoms of Narcolepsy
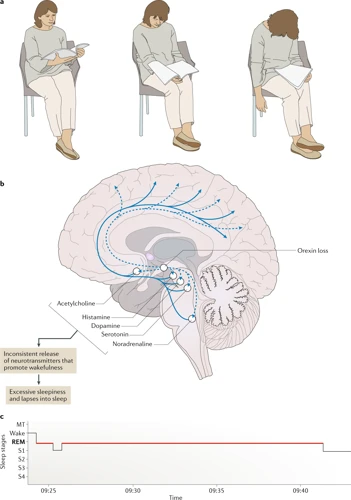
Narcolepsy is a chronic neurological disorder that affects the brain’s ability to regulate sleep-wake cycles, resulting in excessive daytime sleepiness, as well as disturbed nighttime sleep. The symptoms of narcolepsy can vary widely between individuals, but the four primary symptoms are excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations.
Excessive daytime sleepiness is the hallmark symptom of narcolepsy. It is characterized by persistent and overwhelming feelings of sleepiness during the day, regardless of how much sleep a person gets at night. This can make it difficult to complete tasks, concentrate, and stay alert while driving, working, or in social situations.
Cataplexy is a sudden loss of muscle tone that can cause a person to collapse or have trouble moving. It is often triggered by intense emotions such as laughter, anger, or surprise. Some people with narcolepsy may experience mild forms of cataplexy, such as drooping of the eyelids or slurred speech, while others may have more severe episodes of complete muscle paralysis.
Sleep paralysis is a temporary inability to move or speak while falling asleep or waking up. This can be a frightening experience for those who are unaware that it is a symptom of narcolepsy. Sleep paralysis may last for several minutes and can be accompanied by vivid hallucinations.
Hypnagogic hallucinations are dream-like experiences that occur when falling asleep or waking up. They can be vivid and sensory, such as hearing voices, seeing colors, or feeling like someone or something is touching you. They can also be disturbing and frightening, particularly when accompanied by sleep paralysis.
The symptoms of narcolepsy can seriously impact a person’s quality of life, and affect their ability to function normally in daily activities. It is important to seek medical attention if you suspect you may have narcolepsy, as treatment can help manage symptoms and improve quality of life.
Causes of Narcolepsy
The exact causes of narcolepsy are still being studied by researchers, but there are several factors that are believed to play a part in its development. Here are some possible causes of narcolepsy:
- Genetics: There is evidence to suggest that genetics may play a role in the development of narcolepsy. Researchers have identified certain genes that seem to be associated with the disorder, and certain individuals may be more susceptible to developing narcolepsy due to their genetic makeup.
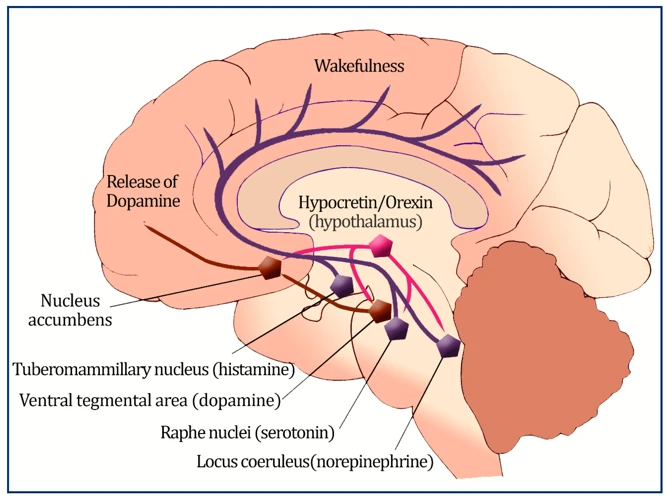
- Neurotransmitters: Narcolepsy may be caused by a deficiency in certain neurotransmitters, which are chemicals that help to transmit signals in the brain. Specifically, low levels of hypocretin, a neurotransmitter that helps to regulate wakefulness, have been linked to the development of narcolepsy.
- Autoimmune Disorders: Some researchers believe that narcolepsy may be an autoimmune disorder, which means that the body’s immune system mistakenly attacks healthy cells in the body. In the case of narcolepsy, the immune system may attack the hypocretin-producing cells in the brain, leading to a deficiency in hypocretin and the development of narcolepsy.
- Brain Injuries: In rare cases, brain injuries or tumors may lead to the development of narcolepsy.
The causes of narcolepsy are still not fully understood, but researchers continue to study the disorder in order to identify the underlying factors that contribute to its development.
Current Research on Narcolepsy
As medical science advances, researchers are constantly delving deeper into the mysteries of narcolepsy – a neurological disorder that causes individuals to experience excessive daytime sleepiness and sudden sleep attacks. Through extensive study, scientists have uncovered a wealth of knowledge about the disorder, including potential genetic and immunological links, as well as the role of various neurotransmitters in its development. In this section, we will highlight the most significant findings from recent research and explore the potential implications for the future of narcolepsy treatment.
Genetics and Narcolepsy
Studies have shown a possible genetic link to narcolepsy, with a higher prevalence among certain populations. More specifically, the HLA-DQB1*06:02 allele has been found to be strongly associated with narcolepsy with cataplexy. Individuals who carry this gene variation are more likely to develop narcolepsy, although it is not a guarantee.
Recent research has also identified other genetic variations that may contribute to the development of narcolepsy. For example, mutations in genes related to the production and regulation of hypocretin (also known as orexin) have been linked to the condition. Hypocretin is a neurotransmitter that plays a crucial role in regulating sleep and wakefulness.
Table: Genetic Factors Associated with Narcolepsy
| Gene or Gene Variation | Function | Association with Narcolepsy |
|---|---|---|
| HLA-DQB1*06:02 | Immune system function | Strongly associated with narcolepsy with cataplexy |
| Hypocretin gene mutations | Hypocretin production and regulation | Linked to the development of narcolepsy |
| TCRA gene | Immune system function | Associated with narcolepsy with cataplexy |
While these genetic variations have been identified as potential risk factors for narcolepsy, it is important to remember that not all individuals with these genetic markers will develop the condition. The interplay between genetics and environmental factors is complex and not fully understood. Further research is needed to fully explore the role of genetics in narcolepsy development.
Neurotransmitters and Narcolepsy
Neurotransmitters play a crucial role in regulating sleep-wake cycles and, therefore, have been the focus of several studies on narcolepsy. One neurotransmitter that has been extensively studied in relation to narcolepsy is hypocretin, also known as orexin, which is produced by cells in the hypothalamus.
Hypocretin in Narcolepsy
Narcolepsy with cataplexy, the most common form of the disorder, is characterized by a deficiency of hypocretin in the brain. Research has shown that individuals with narcolepsy have fewer hypocretin-producing cells in their hypothalamus, which may explain the sudden and uncontrollable sleep attacks associated with the disorder.
Dopamine and Narcolepsy
Dopamine is another neurotransmitter that has been implicated in the development of narcolepsy. Studies have shown that individuals with narcolepsy have lower levels of dopamine in their cerebrospinal fluid, which may contribute to the disorder’s symptoms.
Gamma-Aminobutyric Acid (GABA) and Narcolepsy
GABA is an inhibitory neurotransmitter that helps regulate sleep by reducing neural activity in the brain. Studies have suggested that individuals with narcolepsy may have decreased levels of GABA, which may contribute to the disorder’s symptoms.
| Neurotransmitter | Role in Narcolepsy |
|---|---|
| Hypocretin/orexin | Deficiency in hypocretin production may lead to sleep attacks |
| Dopamine | Lower levels of dopamine may contribute to narcolepsy symptoms |
| Gamma-Aminobutyric Acid (GABA) | Decreased levels of GABA may contribute to narcolepsy symptoms |
Research on neurotransmitters and narcolepsy is ongoing and may lead to new treatments for the disorder in the future.
Immunology and Narcolepsy
Scientists have recently discovered that there may be a relationship between immunology and narcolepsy. Research has shown that in some cases, narcolepsy may be triggered by a combination of genetic and environmental factors that result in an autoimmune response.
Autoimmune Response: An autoimmune response occurs when the immune system mistakenly attacks healthy cells in the body. In narcolepsy, the immune system may target the cells in the brain that produce hypocretin, a neurotransmitter that plays a key role in regulating sleep and wakefulness.
Hypocretin: Hypocretin is a neurotransmitter that is produced by cells in the hypothalamus. It plays a crucial role in regulating sleep and wakefulness by promoting wakefulness and suppressing REM sleep.
HLA Genes: Research has shown that certain genes, known as HLA genes, may be linked to an increased risk of developing narcolepsy. These genes play a key role in regulating the immune system and may be involved in the autoimmune response that causes narcolepsy.
Inflammation: Inflammation may also play a role in the development of narcolepsy. Studies have shown that people with narcolepsy may have higher levels of certain inflammatory markers in their blood, suggesting that inflammation may be involved in the destruction of hypocretin-producing cells in the brain.
Treatment: While there is currently no cure for narcolepsy, researchers are exploring new treatment options that target the immune system. One such treatment is known as intravenous immunoglobulin therapy, which involves infusing the patient with a solution of antibodies collected from healthy donors. This therapy has shown promise in reducing the symptoms of narcolepsy by suppressing the autoimmune response that causes the condition.
The link between immunology and narcolepsy is a relatively new area of research. While it is still not fully understood how the immune system is involved in the development of narcolepsy, there is evidence to suggest that an autoimmune response may be responsible for the destruction of hypocretin-producing cells in the brain. Researchers are hopeful that by better understanding the immune system’s role in narcolepsy, they can develop more effective treatment options for this condition.
Treatments for Narcolepsy
While there is currently no cure for narcolepsy, there are various treatments and strategies available to help manage the symptoms of this chronic sleep disorder. These may involve medications, lifestyle adjustments, and other therapies that aim to improve a person’s quality of life and overall wellbeing. In this section, we’ll explore some of the most common and effective approaches to treating narcolepsy.
Medications for Narcolepsy
The most common medications used to treat narcolepsy symptoms are stimulants, which work by increasing alertness and reducing daytime sleepiness. Some common stimulants used to treat narcolepsy include methylphenidate and amphetamines. Another medication used to treat excessive daytime sleepiness is modafinil, which works differently than traditional stimulants and is less likely to cause jitteriness or anxiety.
In addition to stimulants, another class of medications used to treat narcolepsy are antidepressants. Antidepressants can help improve the symptoms of cataplexy, sleep paralysis, and hallucinations in patients with narcolepsy. Selective serotonin reuptake inhibitors, or SSRIs, are commonly used antidepressants for narcolepsy treatment.
Sodium oxybate is another medication used to treat narcolepsy, specifically to manage cataplexy. This medication is a central nervous system depressant and helps regulate sleep patterns. It is usually taken at night and can improve both nighttime sleep and daytime alertness.
It is important to note that medications for narcolepsy should always be prescribed and monitored by a healthcare professional, as they can have potential side effects and interactions with other medications. Additionally, medications should be used in conjunction with lifestyle changes to manage narcolepsy symptoms effectively.
Lifestyle Changes and Narcolepsy
Making lifestyle changes is an important aspect of managing narcolepsy. It is crucial to maintain a healthy lifestyle to experience the most effective results when dealing with narcolepsy symptoms. Here are some lifestyle changes that can help manage narcolepsy:
- Establish a sleep routine: It is essential to establish a regular sleep routine and get enough sleep, usually seven to eight hours per night. Going to bed and waking up at the same time each day can help regulate the body’s internal clock, leading to improved sleep quality and increased wakefulness.
- Avoid stimulants: Stimulants such as caffeine, nicotine or alcohol can make it difficult to fall asleep or stay asleep, leading to daytime drowsiness. It is important to limit the consumption of these substances, especially at night.
- Take naps: Short naps of 20-30 minutes can help relieve drowsiness and improve alertness during the day. It is essential to schedule naps during the day, as sleeping too late in the afternoon can interfere with nighttime sleep.
- Exercise regularly: Exercise releases endorphins that can help improve mood and relieve symptoms of depression and anxiety, which are common in people with narcolepsy. Regular physical activity can also help improve sleep quality and increase wakefulness.
- Eat a healthy diet: Eating a healthy and balanced diet can help regulate sleep and wake cycles, and improve overall health. Avoiding large meals or foods high in carbohydrates, especially at night, can help prevent drowsiness and sleepiness during the day.
- Avoid working at night: Night shifts can disrupt the natural body clock. People with narcolepsy should avoid working at night or rotating shift schedules if possible, as this can make it difficult to maintain a regular sleep routine.
It is important to remember that each person with narcolepsy may respond differently to lifestyle changes, and it may take some time to find the most effective strategies for managing symptoms. Consistency and perseverance are key to achieving better results.
Conclusion
In conclusion, Narcolepsy is a complex neurological disorder that affects individuals in different ways. It can disrupt daily activities and significantly impact the overall quality of life of affected individuals. Although there is still much research needed to fully understand the causes and mechanisms underlying Narcolepsy, current findings indicate that genetics, neurotransmitters, and immune system dysfunction may all contribute to the disorder.
Thankfully, treatments, such as medication and lifestyle changes, can greatly alleviate the symptoms of Narcolepsy, helping affected individuals lead full and productive lives.
Further research is needed in the future to continue unlocking the mysteries of Narcolepsy and developing more effective treatments. However, with the current understanding and treatment options available, individuals with Narcolepsy can effectively manage their symptoms and improve their quality of life. It is important for healthcare professionals and researchers to continue to work together to find new ways to support those affected by Narcolepsy.
Frequently Asked Questions
What are the different types of narcolepsy?
There are two main types of narcolepsy: Type 1 Narcolepsy with cataplexy and Type 2 Narcolepsy without cataplexy.
Can narcolepsy be genetic?
Yes, it is believed that narcolepsy is often genetically inherited.
How is narcolepsy diagnosed?
Narcolepsy is typically diagnosed through a combination of sleep studies, physical exams, and neurological exams.
What is cataplexy?
Cataplexy is a sudden loss of muscle tone or control, often triggered by strong emotions like laughter or anger.
What neurotransmitter is most commonly associated with narcolepsy?
Orexin, also known as hypocretin, is the neurotransmitter that is most commonly associated with narcolepsy.
Are there any medications that can treat narcolepsy?
Yes, there are several medications that can help manage narcolepsy symptoms, including stimulants and antidepressants.
Is there a cure for narcolepsy?
There is currently no cure for narcolepsy, but symptoms can be managed with medication and lifestyle changes.
Can lifestyle changes help manage narcolepsy symptoms?
Yes, lifestyle changes like maintaining a regular sleep schedule, avoiding alcohol and caffeine, and taking short naps throughout the day can help manage narcolepsy symptoms.
Can narcolepsy affect a person’s ability to work or drive?
Yes, narcolepsy can significantly affect a person’s ability to work or drive safely, especially if they are experiencing excessive daytime sleepiness or sudden bouts of sleep.
Where can I find more information about narcolepsy?
You can find more information about narcolepsy from reputable sources like the National Institute of Neurological Disorders and Stroke, the Narcolepsy Network, and the American Sleep Association.