For many of us, sleep is a time for rest and rejuvenation. However, for those suffering from sleep apnea, this precious time can be fraught with difficulties. Sleep apnea is a disorder that affects the way people breathe while asleep, causing interruptions in breathing patterns and leading to a range of symptoms. But what many people may not realize is that sleep apnea can also have significant impacts on brain health. In this article, we will explore the ways in which sleep apnea affects the brain and examine its links with other health conditions. We will also discuss different treatment options for sleep apnea and the importance of seeking help for this disorder.
What is Sleep Apnea?
Sleep apnea is a perplexing and often misunderstood sleep disorder that affects many people. It can have a significant impact on a person’s overall health, and yet many individuals are not aware that they have it. In this section, we will explore the definition of sleep apnea, the different types of sleep apnea, the causes of sleep apnea, and the common symptoms associated with this condition. By the end, you will have a better understanding of what sleep apnea is and what it entails.
Definition of Sleep Apnea
Sleep apnea is a sleep disorder that causes a person to experience pauses in breathing during sleep. These pauses can last for a few seconds to several minutes, occurring many times throughout the night, and can severely disrupt a person’s sleep, leading to several negative health consequences.
Here are a few key points defining sleep apnea:
- Sleep apnea is a disorder that causes a person to have pauses in breathing or shallow breaths during sleep.
- These pauses can last for as little as a few seconds or as long as several minutes.
- People with sleep apnea may experience breathing cessation dozens or even hundreds of times a night.
Sleep apnea is caused by a variety of factors, including obesity, age, and genetics. It can also be caused by anatomical abnormalities in the upper airway, such as a deviated septum or enlarged tonsils, that restrict airflow.
Here are some factors that can contribute to sleep apnea:
- Being overweight or obese
- Having a thick neck or narrow airway
- Being male
- Being over the age of 40
- Heredity or genetics
- Smoking, alcohol consumption, or use of sedatives or tranquilizers
The development of sleep apnea can lead to several negative health consequences if left untreated, such as high blood pressure, diabetes, and stroke. For this reason, it is important to recognize the symptoms of sleep apnea and seek treatment as soon as possible.
Types of Sleep Apnea
There are two types of sleep apnea, obstructive sleep apnea (OSA) and central sleep apnea (CSA). The table below outlines the main differences between the two types.
| Obstructive Sleep Apnea (OSA) | Central Sleep Apnea (CSA) | |
|---|---|---|
| Definition | A condition in which the airway becomes partially or completely blocked during sleep, leading to breathing pauses and disruptions in sleep. | A condition in which the brain fails to send the proper signals to the muscles that control breathing during sleep. |
| Causes | Obesity, smoking, alcohol use, nasal congestion, and anatomical abnormalities. | Neurological disorders, heart failure, and medications that affect respiratory drive. |
| Symptoms | Loud snoring, gasping or choking during sleep, daytime sleepiness, and morning headaches. | Shortness of breath during sleep, difficulty falling asleep, and frequent awakenings. |
| Treatment | Continuous Positive Airway Pressure (CPAP), oral appliances, surgery, and lifestyle changes. | Treating the underlying cause, such as heart failure or neurological disorders, may improve symptoms. |
It’s important to note that some individuals may have a combination of both types, known as complex sleep apnea syndrome. Proper diagnosis and treatment by a healthcare professional are crucial in managing both types of sleep apnea.
Causes of Sleep Apnea
The causes of sleep apnea are multifactorial and can vary from person to person. Here are some of the common causes:
- Anatomy: People with certain anatomical features such as a small airway or a narrow throat are more prone to sleep apnea. This is because the airway can collapse or become blocked more easily during sleep.
- Obesity: Excess weight can contribute to sleep apnea as it can cause a buildup of fatty tissue that narrows the airway. People with obesity may have decreased muscle tone in the throat, making it more likely to collapse during sleep.
- Age: Sleep apnea can occur at any age, but it is more common in older adults. This may be due to the loss of muscle tone in the throat and the natural aging process that affects the respiratory system.
- Gender: Men are more likely than women to develop sleep apnea, although the reasons for this are not completely understood.
- Family history: Sleep apnea can run in families, suggesting a genetic component.
- Alcohol and sedatives: These substances can relax the muscles in the throat, making it more likely for the airway to collapse during sleep.
- Smoking: Smoking can lead to inflammation and fluid retention in the airway, increasing the risk of sleep apnea.
It is important to note that not everyone who has these risk factors will develop sleep apnea, and not everyone who has sleep apnea will have these risk factors. Consult with a healthcare professional if you suspect that you may have sleep apnea or are experiencing symptoms related to it.
Symptoms of Sleep Apnea
Sleep apnea is a sleep disorder that can adversely affect one’s health. It can cause a host of symptoms that can be alarming to the person experiencing them. Here are some of the most common symptoms of sleep apnea:
- Loud snoring: This is one of the hallmarks of sleep apnea. It can be so loud that it can disturb the sleep of others in the household.
- Pauses in breathing: Sleep apnea can cause a person to stop breathing for several seconds at a time, leading to gasping or choking sounds.
- Frequent waking up: Because of the interruptions in breathing, individuals with sleep apnea may wake up several times throughout the night, though they may not be aware of it.
- Daytime sleepiness: The constant awakenings can leave one feeling fatigued and sleepy during the day, even after what seems to be a full night’s rest.
- Headaches: Headaches, particularly those felt in the morning, can be a sign of sleep apnea.
- Irritability and mood swings: The lack of restful sleep can lead to irritability and frequent mood swings, leaving one feeling drained and overwhelmed.
- Dry mouth or sore throat: Some individuals with sleep apnea may wake up with a dry mouth or sore throat caused by the loud snoring and pauses in breathing.
If you or someone you know experiences one or more of these symptoms, it may be a good idea to seek advice from a healthcare professional. Left untreated, sleep apnea can lead to serious health problems.
Sleep Apnea and Brain Health
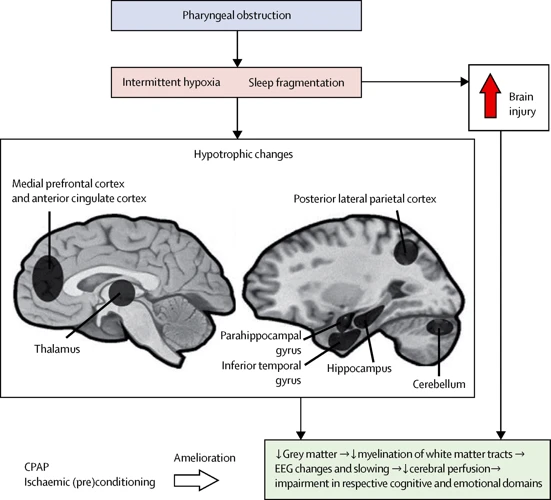
As if struggling with sleep itself wasn’t enough, sleep apnea, a condition that disrupts breathing during sleep, can have a severe impact on the health of the brain. The consequences of sleep apnea can be detrimental to cognitive functioning, as well as increasing the risk of developing neurodegenerative diseases. Understanding how sleep apnea affects the brain can help individuals take proactive steps to manage their condition and improve their overall health.
How Sleep Apnea Affects the Brain
Sleep apnea can have a significant impact on the brain and its functioning. The following are some ways in which sleep apnea affects the brain:
- Insufficient oxygen supply: Sleep apnea can cause oxygen levels in the brain to drop, leading to a condition called hypoxemia. This can damage the brain cells and impair their functioning.
- Disruption of sleep: People with sleep apnea often experience interruptions in their sleep as they awaken briefly to resume their breathing. This can cause daytime sleepiness, lack of concentration, and impaired memory.
- Inflammation: Sleep apnea can also cause inflammation in the brain. This can lead to the destruction of brain cells and increase the risk of a variety of health problems.
- Neurodegeneration: People with sleep apnea have been found to have a greater risk of developing various neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease. This may be due to the damage caused by hypoxemia and inflammation in the brain.
Addressing sleep apnea is vital to preserve brain health and maintain cognitive function. The following section will discuss the impact of sleep apnea on cognitive functioning in greater detail.
Impact of Sleep Apnea on Cognitive Functioning
Sleep apnea can have a significant impact on cognitive functioning. Those who suffer from sleep apnea may experience difficulties with concentration, memory, and decision-making. These issues can affect daily life, work/school performance, and overall quality of life.
The table below highlights the cognitive consequences of untreated sleep apnea:
| Cognitive Functioning | Impact of Sleep Apnea |
|---|---|
| Attention and Concentration | Decreased ability to focus and maintain attention |
| Memory | Difficulty with memory consolidation and retrieval |
| Decision-making | Impaired ability to make effective decisions and solve problems |
These effects can be especially pronounced in individuals with severe sleep apnea. Untreated sleep apnea can lead to microarousals throughout the night, which disrupt sleep and can cause a cycle of daytime sleepiness and cognitive impairment. It is important to seek treatment for sleep apnea in order to improve overall cognitive functioning and quality of life.
Sleep Apnea and Neurodegenerative Diseases
One of the major concerns associated with untreated sleep apnea is the increased risk of neurodegenerative diseases such as Alzheimer’s and Parkinson’s. Multiple studies have found a link between sleep apnea and cognitive decline, further strengthening the need to treat this disorder.
There is evidence that suggests that the frequent interruptions in breathing, experienced by those with sleep apnea, lead to a decrease in oxygen supply to the brain. This lack of oxygen can cause damage to brain cells, and in some cases, can even cause them to die. Over time, this can result in the shrinking of certain areas of the brain, which can impede cognitive functioning.
Studies suggest that individuals with sleep apnea are at greater risk for developing Alzheimer’s disease. A 2017 study published in the Journal of Alzheimer’s Disease found that those with severe sleep apnea were almost three times more likely to develop Alzheimer’s than those without the disorder. Another study published in the Journal of Sleep Research found that sleep apnea is associated with alterations in the connections between brain regions that are involved in memory processing, which is a hallmark symptom of Alzheimer’s disease.
Similarly, research has found a link between sleep apnea and Parkinson’s disease. A 2015 study published in the journal Sleep found that individuals with sleep apnea were more likely to experience a decline in motor skills, which is a common early symptom of Parkinson’s disease. The study also found that those with sleep apnea had a greater risk of developing Parkinson’s disease in the years that followed.
It is important to note that more research is needed to fully understand the relationship between sleep apnea and neurodegenerative diseases. Nonetheless, the increased risk of cognitive decline and neurological disorders is yet another reason why seeking treatment for sleep apnea is crucial for maintaining optimal brain health.
| Neurodegenerative Diseases and Sleep Apnea | Findings |
|---|---|
| Alzheimer’s Disease | Those with severe sleep apnea were almost three times more likely to develop Alzheimer’s than those without the disorder. Sleep apnea is associated with alterations in the connections between brain regions that are involved in memory processing. |
| Parkinson’s Disease | Individuals with sleep apnea were more likely to experience a decline in motor skills, which is a common early symptom of Parkinson’s disease. Those with sleep apnea had a greater risk of developing Parkinson’s disease in the years that followed. |
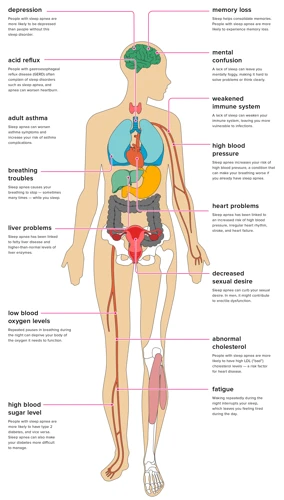
The Link Between Sleep Apnea and Other Health Conditions
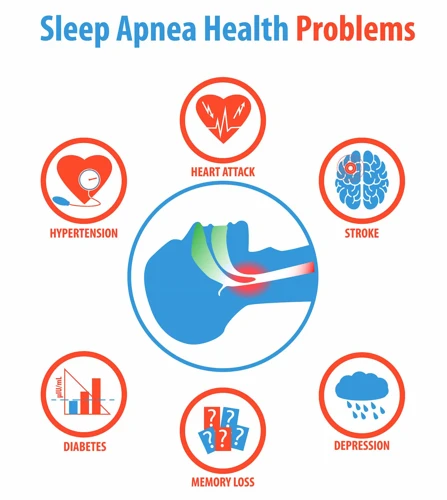
As if the impact on brain health weren’t enough, sleep apnea has also been shown to be associated with a number of other health conditions. From cardiovascular disease to depression and anxiety, the impact of sleep apnea on overall health cannot be ignored. In this section, we will explore the connection between sleep apnea and these various health conditions, highlighting the potential risks and implications for those struggling with sleep apnea.
Cardiovascular Disease
Studies have shown that sleep apnea can significantly increase the risk of developing cardiovascular diseases such as high blood pressure, arrhythmia, stroke, and heart attack. This is due to the fact that the frequent interruptions in breathing during sleep can lead to a decrease in oxygen levels in the blood, which in turn, can cause strain on the cardiovascular system.
High blood pressure: Sleep apnea can cause an increase in blood pressure. This occurs due to the lack of oxygen that occurs during an apneic episode. When the oxygen levels decrease, the sympathetic nervous system is stimulated, leading to an increase in blood pressure. This increase in blood pressure can occur multiple times throughout the night, leading to a sustained increase in blood pressure over time.
Arrhythmia: Sleep apnea has been linked to the development of arrhythmias such as atrial fibrillation. This is due to the fact that the repeated disruptions in breathing can lead to changes in the way the heart beats. The lack of oxygen can also cause electrical instability in the heart, leading to arrhythmias.
Stroke and heart attack: Sleep apnea has been linked to an increased risk of stroke and heart attack. The decrease in oxygen levels that occurs during apneic episodes can cause damage to the blood vessels in the brain and heart. This damage can lead to the formation of blood clots, which can cause stroke or heart attack.
To summarize, sleep apnea can significantly increase the risk of developing cardiovascular diseases such as high blood pressure, arrhythmia, stroke, and heart attack. It is important to address and treat sleep apnea in order to reduce the risk of developing these conditions.
Diabetes
Sleep apnea has also been linked to diabetes, a chronic condition that affects how the body processes blood sugar. The relationship between sleep apnea and diabetes is bidirectional, meaning that each condition can worsen the other.
On one hand, sleep apnea can increase the risk of developing diabetes by disrupting the body’s hormonal balance and causing insulin resistance. Over time, these effects can make it harder for the body to use insulin properly, leading to high blood sugar levels and an increased risk of developing type 2 diabetes.
On the other hand, diabetes can worsen the symptoms of sleep apnea, making it more difficult to manage. High glucose levels can damage the nerves that control breathing, leading to breathing difficulties at night. Additionally, people with diabetes are more likely to have obesity or other comorbidities that can contribute to sleep apnea.
To make matters worse, poor sleep quality has been linked to worsening of insulin resistance in people with diabetes, meaning that sleep apnea can exacerbate the metabolic dysfunction associated with the condition.
In fact, studies have found that treating sleep apnea in people with diabetes can lead to improvements in blood sugar control and insulin sensitivity. This emphasizes the importance of addressing sleep apnea in people with diabetes, as it may help to improve their overall health outcomes.
Table: The Relationship Between Sleep Apnea and Diabetes
| Sleep Apnea | Diabetes |
|---|---|
| Can increase the risk of developing diabetes | Can worsen the symptoms of sleep apnea |
| Can disrupt the body’s hormonal balance and cause insulin resistance | Can damage the nerves that control breathing, leading to breathing difficulties at night |
| Can exacerbate the metabolic dysfunction associated with diabetes | Poor sleep quality linked to worsening of insulin resistance in people with diabetes |
| Treating sleep apnea can lead to improvements in blood sugar control and insulin sensitivity in people with diabetes |
It is essential to screen for and treat sleep apnea in people with diabetes to reduce the risk of complications and improve overall health outcomes.
Depression and Anxiety
Studies have shown a strong link between sleep apnea and mental health issues, particularly depression and anxiety. Sleep disruptions caused by sleep apnea can exacerbate or even trigger these conditions.
Research has shown that people with sleep apnea are more likely to experience symptoms of depression, such as persistent feelings of sadness, hopelessness, and loss of interest in daily activities. Those with untreated sleep apnea are at higher risk of developing clinical depression.
Anxiety is another common mental health issue associated with sleep apnea. Those with untreated sleep apnea are more likely to experience symptoms of anxiety, such as excessive worry and fear about everyday situations.
In fact, the link between sleep apnea and mental health issues can create a vicious cycle, where the negative impact of poor sleep on mental health creates more stress, which in turn exacerbates sleep apnea symptoms.
| Issue | Symptoms |
|---|---|
| Depression | Persistent sadness, hopelessness, loss of interest in daily activities. |
| Anxiety | Excessive worry and fear about everyday situations. |
It is important to address both the sleep apnea and the mental health issues in order to break this cycle. This can be done through a variety of means, including therapy, medication, and sleep apnea treatment such as continuous positive airway pressure (CPAP) therapy or oral appliances.
By seeking treatment for both sleep apnea and mental health issues, individuals can improve their overall quality of life and reduce the risk of developing further health complications.
Treatment for Sleep Apnea
Finding the right treatment for sleep apnea can be perplexing, but it’s essential for managing the condition and improving your overall health. Treatment options range from lifestyle changes to corrective surgery, and it’s important to work with a healthcare professional to determine the best approach for your specific needs. In this section, we’ll explore the various treatment options available for sleep apnea, including continuous positive airway pressure (CPAP), oral appliances, surgery, and lifestyle changes.
Continuous Positive Airway Pressure (CPAP)
One of the most effective treatments for sleep apnea is Continuous Positive Airway Pressure (CPAP). This therapy works by providing a constant flow of air pressure through a mask worn over the nose and/or mouth during sleep. The air pressure helps to keep the airway open and prevent episodes of apnea or hypopnea.
Advantages of CPAP therapy
CPAP therapy has numerous advantages, some of which include:
| Advantages of CPAP therapy |
|---|
| Improves quality of sleep |
| Reduces daytime sleepiness and fatigue |
| Reduces snoring |
| Reduces the risk of developing other health problems associated with sleep apnea |
Types of CPAP machines
There are several types of CPAP machines available, each with its own unique features. Some of the most common types include:
| Type of CPAP machine | Description |
|---|---|
| Standard CPAP machine | Provides a fixed air pressure throughout the night |
| Bi-level positive airway pressure (BiPAP) machine | Provides two different levels of air pressure: a higher level when inhaling and a lower level when exhaling |
| Automatic positive airway pressure (APAP) machine | Adjusts the air pressure based on the patient’s breathing patterns throughout the night |
| Travel CPAP machine | Lightweight and portable, designed for use while travelling |
CPAP compliance
One of the potential drawbacks of CPAP therapy is that it requires the patient to wear a mask over their face throughout the night. This can take some getting used to, and some patients may find it uncomfortable or difficult to sleep with the mask on.
It’s important to note that CPAP therapy is only effective if the patient uses the machine as directed. This means wearing the mask for the entire night every night. Failure to comply with therapy can lead to a worsening of sleep apnea symptoms and an increased risk of associated health problems.
CPAP therapy is a highly effective treatment for sleep apnea that can provide numerous benefits for patients who use it as directed.
Oral Appliances
One of the most common and effective treatments for sleep apnea is the use of oral appliances. These are devices that are worn in the mouth during sleep to help keep the airway open and reduce the frequency and severity of apneas.
There are several types of oral appliances, which can be custom-made by a dentist or purchased over-the-counter. Some of the most commonly used devices include:
| Type of Oral Appliance | How It Works |
|---|---|
| Mandibular Advancement Device (MAD) | This device looks like a mouthguard and is designed to hold the lower jaw forward to open up the airway. |
| Tongue-Retaining Device (TRD) | This device uses a suction cup to hold the tongue in place, preventing it from blocking the airway during sleep. |
| Pillows or Straps | These devices position the head and neck in a way that helps keep the airway open. |
Oral appliances are generally more comfortable and easier to use than continuous positive airway pressure (CPAP) machines, which are another common treatment for sleep apnea. However, they may not be as effective for severe cases of sleep apnea.
If you are considering oral appliance therapy, it is important to consult with a dentist or sleep specialist who can help determine the best type of device for your individual needs. They can also provide instructions on how to properly use and care for the appliance to ensure its effectiveness and longevity.
Surgery
Surgery is another option for treating sleep apnea, but it is usually only recommended if other treatments have failed or if there is a clear physical abnormality causing the sleep apnea. The specific type of surgery recommended will depend on the individual’s case and the cause of their sleep apnea.
Common types of surgeries for sleep apnea include:
| Surgery Type | Description |
|---|---|
| Uvulopalatopharyngoplasty (UPPP) | A surgery that removes excess tissue from the throat, including the uvula, tonsils, and part of the soft palate, to widen the airway. |
| Maxillomandibular advancement (MMA) | A surgery that moves the upper and lower jaw forward to increase the airway space. |
| Nasal surgery | A surgery that corrects any nasal abnormalities or blockages that could be contributing to sleep apnea. |
| Tracheostomy | A surgery that creates a new opening in the neck to bypass the blocked airway. This is typically only recommended for severe cases of sleep apnea when other treatments have failed. |
It is important to note that surgery can have risks and potential side effects, and it may not completely cure sleep apnea. It is important to discuss the pros and cons of surgery with a medical professional before making a decision. Additionally, lifestyle changes such as weight loss or quitting smoking may also be recommended to improve the success of surgery and overall health.
Lifestyle Changes
Making certain lifestyle changes can significantly improve sleep quality and reduce the symptoms of sleep apnea. Here are some changes that can make a difference:
- Weight loss: Excess weight, particularly around the neck, can cause obstructions in the airway, leading to sleep apnea. Losing weight through healthy eating and exercise can reduce the severity of sleep apnea.
- Regular exercise: Regular physical activity can also help manage sleep apnea. Exercise can help with weight loss and reduce stress, leading to better sleep. Aim for at least 30 minutes of moderate physical activity most days of the week.
- Healthy sleep habits: Establishing a regular sleep routine and maintaining good sleep hygiene can improve sleep quality. This includes going to bed and waking up at the same time each day, avoiding electronic devices before bedtime, and creating a comfortable sleep environment.
- Avoiding alcohol and sedatives: Alcohol and sedatives can relax the muscles in the throat, exacerbating sleep apnea symptoms. Avoid these substances, particularly before bedtime.
- Sleeping on your side: Sleeping on your back can make sleep apnea symptoms worse by allowing gravity to push the throat muscles and tongue back. Sleeping on your side can prevent this.
- Quitting smoking: Tobacco use can cause inflammation and swelling in the airway, exacerbating the symptoms of sleep apnea. Quitting smoking can improve overall health and reduce sleep apnea symptoms.
Making lifestyle changes can be challenging, but they can lead to significant improvements in sleep quality and overall health. Consult with a healthcare provider to determine which changes are most appropriate for you.
Conclusion
In conclusion, sleep apnea is a serious sleep disorder that can have negative effects on brain health and overall well-being. It is important to recognize the symptoms of sleep apnea and seek medical attention for proper diagnosis and treatment.
Continuous Positive Airway Pressure (CPAP), oral appliances, surgery, and lifestyle changes can all be effective treatments for sleep apnea. However, it is essential to consult with a healthcare professional to determine the best course of action.
Ignoring the symptoms of sleep apnea can lead to a variety of health issues, including cardiovascular disease, diabetes, depression, and anxiety. In addition, sleep apnea may also increase the risk of developing neurodegenerative diseases such as Alzheimer’s and dementia.
It is crucial to prioritize getting enough timely and quality sleep and to hold accountable for a healthy and sustainable lifestyle to maintain overall physical and mental health. If you or your loved one is struggling with sleep apnea, do not hesitate to reach out to your healthcare provider for support and guidance.
Frequently Asked Questions
Can sleep apnea be cured?
There is no guaranteed cure for sleep apnea, but it can be effectively managed through various treatment options.
Does sleep apnea only affect older adults?
No, sleep apnea can affect people of all ages, including children.
What is the best treatment for sleep apnea?
The best treatment for sleep apnea varies depending on the severity and underlying cause, but options can include CPAP therapy, oral appliances, surgery, and lifestyle changes.
What are the long-term health risks of untreated sleep apnea?
Untreated sleep apnea can increase the risk of developing cardiovascular disease, diabetes, depression, and neurodegenerative diseases.
Is snoring always a sign of sleep apnea?
No, snoring can be a symptom of sleep apnea, but not everyone who snores has sleep apnea.
Can sleep apnea cause memory loss?
Yes, sleep apnea can impact cognitive functioning, including memory, due to disrupted sleep and decreased oxygenation to the brain.
Is weight loss an effective treatment for sleep apnea?
Weight loss can be an effective treatment for sleep apnea, particularly for those with obstructive sleep apnea, as excess weight can contribute to airway obstruction.
Can alcohol consumption worsen sleep apnea symptoms?
Yes, alcohol can relax the muscles in the throat, making it more difficult to breathe during sleep and exacerbating sleep apnea symptoms.
What is positional therapy for sleep apnea?
Positional therapy involves training the body to sleep in a position that reduces the likelihood of airway obstruction, such as sleeping on one’s side rather than the back.
What can happen if sleep apnea goes untreated?
Untreated sleep apnea can lead to chronic fatigue, increased risk of accidents and injuries, and a range of long-term health complications.