Living with Narcolepsy can be a daily challenge for anyone who experiences the symptoms of this neurological disorder. The condition is characterized by excessive daytime sleepiness, sudden bouts of sleep, and even muscle weakness or paralysis triggered by strong emotions. For those who struggle with Narcolepsy, finding effective treatments can be a vital step towards managing their symptoms and improving their quality of life. In this article, we will explore the medications and therapies that are commonly used to treat Narcolepsy, including the benefits and potential side effects associated with each type of treatment.
Medications for Narcolepsy
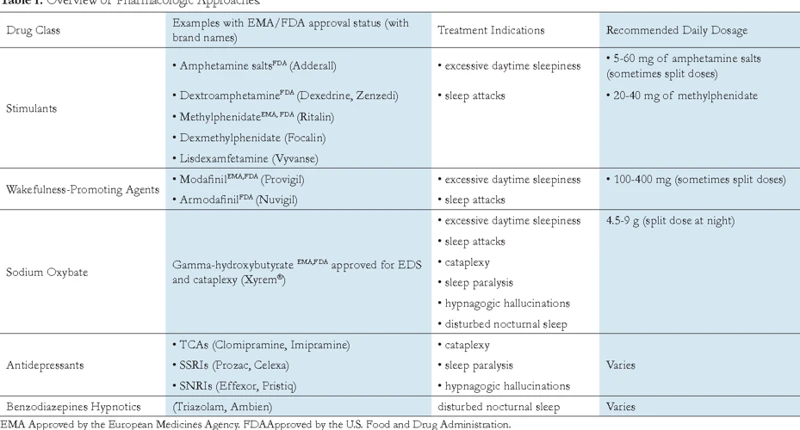
For those struggling with narcolepsy, medications can be a crucial component in managing their symptoms. There are several different types of medications available, each with their own benefits and drawbacks. From stimulants that help combat excessive daytime sleepiness to Selective Serotonin Reuptake Inhibitors (SSRIs) that can improve symptoms of cataplexy, choosing the right medication can make all the difference in the quality of life of someone with narcolepsy. Let’s take a closer look at the various options available.
Stimulants
Stimulants are the most commonly prescribed medications for narcolepsy. They work by increasing levels of dopamine and norepinephrine in the brain, which can help to reduce excessive daytime sleepiness and improve alertness. Some examples of stimulants used to treat narcolepsy include:
- Methylphenidate: This medication is a central nervous system (CNS) stimulant that is often used to treat attention deficit hyperactivity disorder (ADHD). It can also be effective in reducing excessive daytime sleepiness in people with narcolepsy.
- Modafinil: This medication is a CNS stimulant that is FDA-approved to treat excessive daytime sleepiness associated with narcolepsy. It has been shown to improve wakefulness and reduce fatigue in people with narcolepsy.
- Armodafinil: This medication is a newer version of modafinil that is longer-lasting and may be more effective in promoting wakefulness.
- Dexmethylphenidate: This medication is another CNS stimulant that is commonly used to treat ADHD. It can also be used to reduce excessive daytime sleepiness in people with narcolepsy.
While stimulants can be effective in reducing excessive daytime sleepiness, they can also have side effects, such as insomnia, nervousness, and increased heart rate. It is important to work closely with a healthcare provider to identify the most appropriate medication and dosage for an individual’s needs. Additionally, it is important to use stimulants as directed and not to exceed the recommended dosage.
Sodium Oxybate (Xyrem)
Sodium Oxybate, also known as Xyrem, is a medication approved by the FDA for the treatment of narcolepsy with cataplexy in adults. It is a central nervous system depressant and has sedative effects, making it effective in reducing excessive daytime sleepiness (EDS) and cataplexy.
Xyrem is a sodium salt of gamma-hydroxybutyrate (GHB), which is a naturally occurring neurochemical in the brain. It is taken twice per night, typically 2.5-4 hours apart. The first dose is taken at bedtime, and the second is taken during the night to help improve nighttime sleep continuity. It is important to follow the dosing instructions carefully, as taking too much can lead to serious side effects.
| Pros | Cons |
| – Effective in reducing EDS and cataplexy | – Can cause side effects such as nausea, dizziness, and headache |
| – Can improve nighttime sleep quality | – Requires strict adherence to dosing instructions |
| – Can improve overall quality of life for those with narcolepsy with cataplexy | – Only approved for use in adults |
Xyrem is a controlled substance due to its potential for abuse and misuse. It should only be used under the supervision of a healthcare provider and should never be shared with others. While Xyrem can be an effective treatment for narcolepsy with cataplexy, it is important to weigh the potential benefits against the risks and carefully follow dosing instructions to minimize the risk of side effects.
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective Serotonin Reuptake Inhibitors (SSRIs) are a type of medication that can be used to treat the symptoms of narcolepsy. These medications work by increasing the amount of serotonin available in the brain, which can help with sleep regulation.
Examples of SSRIs include:
- Fluoxetine (Prozac)
- Paroxetine (Paxil, Pexeva)
- Sertraline (Zoloft)
SSRIs are often used in combination with other medications, such as stimulants, to manage the symptoms of narcolepsy. They can also be used to treat depression and anxiety, which are common comorbidities of narcolepsy.
It’s important to note that SSRIs can have potential side effects, such as nausea, dizziness, and sexual dysfunction. It’s important to discuss any potential side effects with a healthcare provider before starting this type of medication.
SSRIs may also interact with other medications, so it’s important to disclose all medications currently being taken to a healthcare provider.
SSRIs can be a useful tool in managing the symptoms of narcolepsy, particularly when used in combination with other medications and therapies. However, it’s important to work closely with a healthcare provider to determine the best treatment plan for each individual.
Tricyclic antidepressants (TCAs)
Tricyclic antidepressants (TCAs) are a class of medications that can be used to treat narcolepsy. These medications affect the levels of certain neurotransmitters in the brain, including serotonin and norepinephrine. Some common TCAs used for narcolepsy include imipramine, desipramine, and protriptyline.
- How do TCAs work? TCAs work by blocking the reuptake of certain neurotransmitters in the brain. This increases the levels of these neurotransmitters, which can help improve daytime sleepiness and cataplexy in people with narcolepsy.
- What are the benefits of TCAs? TCAs can be effective at reducing daytime sleepiness and cataplexy in people with narcolepsy. They can also improve mood and reduce anxiety and depression, which are common comorbidities of narcolepsy.
- What are the potential side effects of TCAs? Common side effects of TCAs include dry mouth, constipation, blurred vision, dizziness, and weight gain. More serious side effects can include heart arrhythmias, seizures, and liver damage. TCAs may also interact with other medications or substances, so it’s important to speak with your doctor about any other medications you’re taking before starting a TCA for narcolepsy.
- Who may benefit from TCAs? TCAs may be particularly effective for people with narcolepsy who also struggle with mood disorders or anxiety. They may also be a good option for people who do not respond well to other medications or who cannot tolerate the side effects of other medications.
It’s important to note that TCAs can take several weeks to begin working, and they should be taken under the guidance of a healthcare provider. They may also interact with other medications or substances, so it’s important to speak with your doctor about any other medications you’re taking before starting a TCA for narcolepsy.
Other medications
In addition to stimulants, sodium oxybate (Xyrem), selective serotonin reuptake inhibitors (SSRIs), and tricyclic antidepressants (TCAs), there are other medications that can be used in the treatment of narcolepsy.
One such medication is Modafinil, which is a wakefulness-promoting agent. It works by altering the levels of certain neurotransmitters in the brain, including dopamine, norepinephrine, and histamine. Modafinil has been found to improve wakefulness and reduce excessive daytime sleepiness in people with narcolepsy.
Another medication that can be used is Armodafinil. Like Modafinil, it is a wakefulness-promoting agent that alters the levels of certain neurotransmitters in the brain. It has been shown to be effective in reducing excessive daytime sleepiness in people with narcolepsy.
Antidepressants are another class of medications that can be used in the treatment of narcolepsy. While SSRIs and TCAs are commonly used, other types of antidepressants may also be prescribed. For example, bupropion is an antidepressant that has been found to reduce symptoms of daytime sleepiness in people with narcolepsy.
Finally, Anticataplectic agents may be used to treat narcolepsy with cataplexy. These medications are specifically aimed at reducing or eliminating the symptoms of cataplexy, which is a sudden loss of muscle tone often triggered by emotional responses. Examples of anticataplectic agents include sodium oxybate, venlafaxine, and clomipramine. It’s important to note that these medications may have side effects and should only be used under the guidance of a healthcare professional.
Therapies for Narcolepsy
Individuals with narcolepsy often struggle with excessive daytime sleepiness, sudden sleep attacks, and other debilitating symptoms. While medications can help manage these symptoms, they may not be enough on their own. That’s where therapies for narcolepsy come in. These additional treatments can be crucial for improving quality of life and reducing the impact of narcolepsy on daily routines. Some focus on supporting wakefulness during the day, while others address specific symptoms like cataplexy. Let’s explore some of the most effective therapies for narcolepsy.
Nap therapy
Nap therapy is a common treatment for narcolepsy. It involves taking short naps throughout the day to help reduce excessive daytime sleepiness. These naps are typically 15 to 20 minutes long and spaced out at regular intervals, usually every few hours.
Nap therapy can be done on its own or in combination with medication. It can also be customized to fit an individual’s schedule and specific needs. For example, some people may benefit from longer or more frequent naps, while others may find that shorter or less frequent naps are effective.
The effectiveness of nap therapy may vary from person to person, but many people with narcolepsy find it to be a helpful tool in managing their symptoms. It can be particularly beneficial for those who experience sudden sleep attacks or who have difficulty staying awake during important activities like driving or working.
It’s important to note that nap therapy may not be feasible for everyone due to work or other life obligations. Additionally, it may not provide complete symptom relief for some individuals with narcolepsy.
Nap therapy can be a valuable treatment option for narcolepsy, particularly when used in combination with other therapies and lifestyle changes. The following table summarizes the key points of nap therapy:
| Nap Therapy for Narcolepsy | |
|---|---|
| Description | Taking short naps throughout the day to reduce excessive daytime sleepiness. |
| Length of Naps | Typically 15 to 20 minutes. |
| Frequency of Naps | Spaced out at regular intervals, usually every few hours. |
| Customizability | Can be customized to fit an individual’s schedule and specific needs. |
| Effectiveness | May vary from person to person, but many people with narcolepsy find it to be a helpful tool in managing their symptoms. |
| Potential Limitations | May not be feasible for everyone due to work or other life obligations. It may not provide complete symptom relief for some individuals with narcolepsy. |
Cognitive behavioral therapy (CBT)
Cognitive behavioral therapy (CBT) is based on the idea that one’s thoughts, feelings, and behaviors are interconnected. CBT aims to identify negative thought patterns that may be contributing to narcoleptic symptoms and then aims to change them through a combination of techniques. These techniques can include:
- Education: Therapists can educate patients about narcolepsy to help them better understand their condition and ways to cope with symptoms.
- Sleep hygiene: Therapists can teach patients ways to improve their sleep quality, such as sticking to a consistent sleep schedule, avoiding caffeine and alcohol, and keeping the bedroom dark and quiet.
- Relaxation techniques: These can include deep breathing exercises, progressive muscle relaxation, and meditation. These techniques can help patients manage stress, which can exacerbate narcoleptic symptoms.
- Cognitive restructuring: This involves identifying and challenging negative thought patterns, such as catastrophizing (expecting the worst) and all-or-nothing thinking. Therapists can help patients develop more balanced and realistic ways of thinking, which can reduce anxiety and improve mood.
- Behavioral activation: This approach focuses on increasing engagement in positive activities and decreasing avoidance behaviors, such as staying in bed all day due to fatigue or anxiety. Therapists can help patients identify enjoyable and meaningful activities and develop a plan for incorporating them into their daily routine.
CBT can be delivered in individual or group settings, and typically involves weekly sessions for several months. It has been shown to be effective in improving sleep quality, reducing daytime sleepiness, and improving mood in people with narcolepsy. Additionally, CBT can be used in combination with medications for maximal symptom relief.
Third Wave CBT
Third Wave Cognitive Behavioral Therapy (CBT) is another type of therapy that has proven to be effective in managing narcolepsy symptoms. This kind of therapy works by using mindfulness, acceptance, and values-based techniques to help individuals living with narcolepsy manage their symptoms and improve their quality of life.
Mindfulness is about staying focused on the present moment and becoming more aware of physical sensations, thoughts, and emotions. It can be useful for narcolepsy patients who are experiencing anxiety or depression due to their condition.
Acceptance involves learning to accept one’s strengths and limitations, including the symptoms of narcolepsy. By embracing the reality of their condition, individuals can learn to live with it and manage it.
Values-based techniques help individuals to align their behavior with their personal values. This can help them to prioritize what is important in their lives and create a sense of purpose.
Third Wave CBT seeks to help individuals living with narcolepsy to better understand their condition and learn new coping mechanisms. By cultivating mindfulness, acceptance, and values-based techniques, it can be a powerful tool in managing the symptoms of narcolepsy and improving one’s overall quality of life.
Cataplexy-focused therapy
One type of therapy that specifically targets cataplexy in narcolepsy patients is called cataplexy-focused therapy. This therapy aims to help individuals identify triggers and emotional states that may lead to a cataplexy attack, and to develop strategies for avoiding those triggers or handling them more effectively when they do arise. Here are some of the techniques that may be used in cataplexy-focused therapy:
- Social support: Often, individuals with narcolepsy feel isolated or ashamed about their condition, especially when coping with episodes of cataplexy. Cataplexy-focused therapy can involve working with a therapist or support group to develop a sense of community and connection, which can help to reduce feelings of shame or embarrassment.
- Mindfulness techniques: Some therapies may focus on mindfulness techniques such as meditation or deep breathing exercises to help patients stay aware of their emotional states and develop a sense of control over their body during an attack.
- Muscle relaxation: Techniques such as progressive muscle relaxation or yoga may be used to help patients become more attuned to their physical signs of cataplexy and develop better control over their muscles during an attack.
- Exposure therapy: In some cases, cataplexy-focused therapy may involve gradually exposing patients to stimuli that typically trigger a cataplexy attack in order to help them build up a tolerance over time and reduce the severity of future episodes.
Cataplexy-focused therapy can be a valuable tool for minimizing the impact of cataplexy on a patient’s daily life and improving their sense of control over their condition. By working with a therapist to identify and address the underlying emotional and physical factors that contribute to cataplexy attacks, individuals with narcolepsy can reduce the frequency and severity of their symptoms and live a more fulfilling life.
Lifestyle changes
In addition to medications and therapies, lifestyle changes can also play a crucial role in managing narcolepsy symptoms. Here are some important changes that can help:
- Establish a regular sleep schedule: Maintaining a consistent sleep schedule by going to bed and waking up at the same time every day, even on weekends, can help regulate your body’s sleep-wake cycle and improve daytime alertness.
- Avoid sleep-depriving activities: Avoid activities that can reduce your sleep, such as working or studying late, watching TV in bed, or using electronic devices before bedtime.
- Create a sleep-conducive environment: Ensure that your bedroom is conducive to sleep by keeping it comfortable, quiet, cool, and dark.
- Take naps: Short naps during the day can help you feel more alert and refreshed. Try to limit naps to 20-30 minutes to avoid disrupting your nighttime sleep.
- Eat a healthy diet: A healthy diet rich in fruits, vegetables, whole grains, and lean protein can help promote daytime alertness.
- Avoid alcohol and caffeine: Alcohol and caffeine can disrupt sleep and lead to daytime drowsiness, so it’s important to avoid or limit these substances.
- Exercise regularly: Regular exercise can improve overall health and promote better sleep quality, which can help with daytime alertness.
- Manage stress: Stress can interfere with sleep quality and exacerbate narcolepsy symptoms, so it’s important to find healthy ways to manage stress, such as meditation, yoga, or deep breathing exercises.
By incorporating these lifestyle changes into your daily routine, you can effectively manage your narcolepsy symptoms and enjoy a better quality of life.
Conclusion
In conclusion, narcolepsy is a chronic neurological disorder that can significantly impact an individual’s daily life. However, there are various treatment options available to manage symptoms effectively. Medications such as stimulants and Sodium Oxybate (Xyrem) can help with excessive daytime sleepiness and cataplexy. Selective Serotonin Reuptake Inhibitors (SSRIs) and Tricyclic antidepressants (TCAs) have also shown promising results in managing symptoms.
Aside from medications, various therapies can also be beneficial in managing narcolepsy symptoms. Nap therapy, cognitive behavioral therapy (CBT), third-wave CBT, cataplexy-focused therapy, and lifestyle changes such as creating a regular sleep schedule and exercise can significantly improve an individual’s quality of life.
It is important to note that treating narcolepsy can be challenging as it requires a personalized approach. Therefore, a healthcare professional who specializes in sleep disorders should be consulted to determine the most effective treatment plan. With the right treatment and lifestyle changes, individuals with narcolepsy can manage their symptoms and enjoy a fulfilling life.
Frequently Asked Questions
What causes narcolepsy?
The exact cause of narcolepsy is still unknown, but it is believed to involve genetic and environmental factors that lead to a loss of brain cells that produce the neurotransmitter hypocretin.
What are the symptoms of narcolepsy?
The main symptoms of narcolepsy are excessive daytime sleepiness, sudden and uncontrollable sleep attacks, sleep paralysis, and hallucinations.
How is narcolepsy diagnosed?
Narcolepsy is usually diagnosed with a combination of a physical exam, sleep study, and a medical history review. A special blood test can also help confirm a diagnosis.
Are there any medications that can treat narcolepsy?
Yes, there are a variety of medications that can help manage narcolepsy symptoms. These include stimulants, sodium oxybate, SSRIs, TCAs, and other drugs.
Can lifestyle changes help manage narcolepsy symptoms?
Yes, lifestyle changes such as maintaining a regular sleep schedule, avoiding caffeine and alcohol, and taking short naps during the day can all help manage narcolepsy symptoms.
Is there a cure for narcolepsy?
Unfortunately, there is no cure for narcolepsy at this time. However, treatments and therapies can help manage symptoms and improve quality of life.
What is cognitive behavioral therapy?
Cognitive behavioral therapy (CBT) is a form of therapy that focuses on identifying and changing negative thought patterns and behaviors. It can be helpful in managing narcolepsy symptoms such as anxiety and depression.
What is third wave CBT?
Third wave CBT is a newer form of cognitive behavioral therapy that incorporates mindfulness and acceptance-based techniques. It may be helpful for managing narcolepsy symptoms along with traditional CBT.
What is cataplexy?
Cataplexy is a sudden loss of muscle tone that is often triggered by strong emotions such as laughter, anger, or surprise. It is a common symptom of narcolepsy and can be managed with medication and therapy.
Can narcolepsy be fatal?
Narcolepsy itself is not usually fatal, but the symptoms can be dangerous in certain situations such as when driving or operating heavy machinery. It is important to properly manage symptoms to avoid accidents.