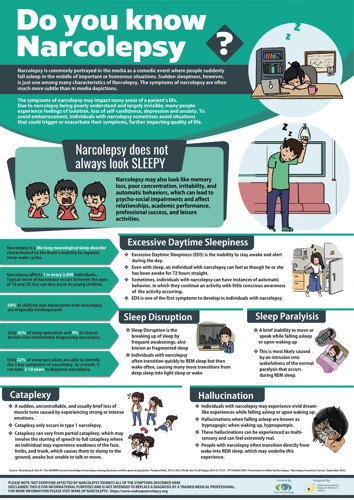
Have you ever heard of a condition where a person goes from being wide awake to suddenly falling into a deep sleep within seconds? This baffling disorder is called narcolepsy. It’s a neurological disorder that affects the body’s sleep-wake cycles, leading to sudden bouts of sleepiness and uncontrollable sleep episodes during the day. People with narcolepsy often experience symptoms such as excessive daytime sleepiness, sleep paralysis, and hallucinations. In this article, we’ll take a closer look at the symptoms and causes of narcolepsy, the different types of narcolepsy, how narcolepsy is diagnosed and treated, as well as the various complications and risks associated with this condition.
What is Narcolepsy?

Narcolepsy is a rare sleep disorder that affects the way an individual’s brain regulates sleep-wake cycles. Those who suffer from narcolepsy have an overwhelming, uncontrollable desire to sleep at various times throughout the day, regardless of how much sleep they may have had the night before. These sudden attacks of extreme sleepiness can occur at any time, even while driving or in the middle of a conversation. Individuals with narcolepsy often experience muscle weakness or paralysis, hallucinations, and disrupted nighttime sleep. Let’s explore the symptoms and causes of this perplexing disorder.
Symptoms of Narcolepsy
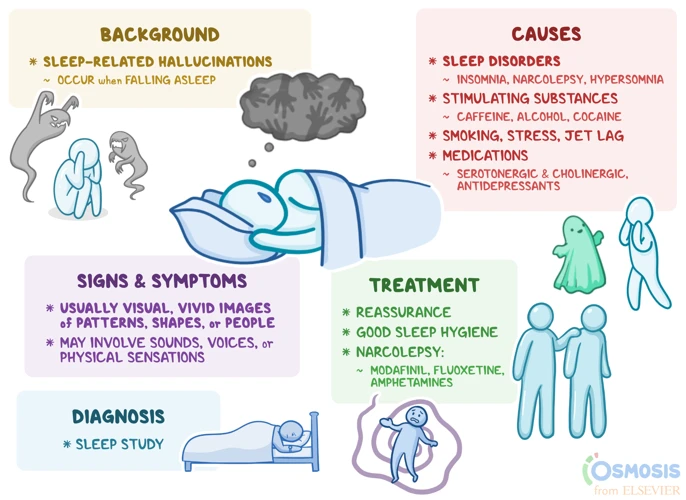
Narcolepsy is a chronic neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. People with narcolepsy may experience a wide range of symptoms, which can significantly impact their daily life.
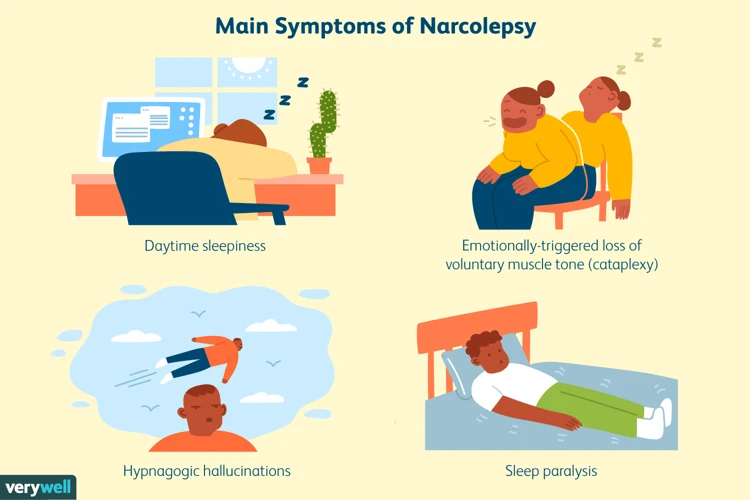
The primary symptoms of narcolepsy include excessive daytime sleepiness (EDS), cataplexy, sleep paralysis, hallucinations, and disrupted nighttime sleep. These symptoms can vary in severity and frequency from person to person.
Narcolepsy symptoms are often mistaken for other conditions, such as depression, anxiety, or sleep apnea. It is important to consult a healthcare professional if you experience any of the following symptoms:
| Symptom | Description |
|---|---|
| Excessive Daytime Sleepiness (EDS) | Feeling drowsy or falling asleep during the day, even after a full night’s sleep. |
| Cataplexy | Sudden loss of muscle tone triggered by strong emotions, such as laughter or anger. |
| Sleep Paralysis | Temporary inability to move or speak while falling asleep or waking up. |
| Hallucinations | Vivid, often frightening, sensory experiences while falling asleep or waking up. |
| Disrupted Nighttime Sleep | Difficulty falling or staying asleep, frequent awakenings, and vivid dreams or nightmares. |
Additionally, some people with narcolepsy may experience secondary symptoms, such as automatic behavior, in which they continue to perform routine tasks while asleep or half-awake, or a reversed sleep-wake cycle, in which they are more alert and awake at night and sleep during the day.
It is important to note that not all people with narcolepsy will experience all of these symptoms, and some symptoms may be more severe than others. The severity of symptoms may fluctuate over time, making it difficult to manage daily life activities.
Causes of Narcolepsy
Narcolepsy is a sleep disorder that affects the nervous system. The causes of narcolepsy are not fully understood, but experts believe that it is caused by a combination of genetic and environmental factors. Here are some potential causes of narcolepsy:
- Genetic predisposition: Research suggests that there may be a genetic component to narcolepsy. Studies have found that individuals with narcolepsy are more likely to have a family member with the condition compared to those without narcolepsy.
- Autoimmune dysfunction: Another potential cause of narcolepsy is an autoimmune dysfunction. This is a condition in which the immune system mistakenly attacks healthy cells in the body. In narcolepsy, the immune system targets cells in the brain that produce hypocretin, a neurotransmitter that helps regulate wakefulness and REM sleep.
- Brain injury or trauma: In rare cases, narcolepsy may be caused by brain injury or trauma. This may include head trauma, stroke, or brain tumors.
- Infections: Some infections, such as streptococcal infection, may be a trigger for narcolepsy in some individuals.
- Exposure to toxins: Exposure to toxins, such as pesticides or chemicals, may also be a potential cause of narcolepsy.
While the exact cause of narcolepsy is still being researched, understanding potential factors that contribute to its development can help individuals manage their condition more effectively.
Types of Narcolepsy
When it comes to narcolepsy, it’s not a one-size-fits-all condition. In fact, there are different types of narcolepsy that affect individuals in varying ways. Understanding the nuances between these types can be crucial in effectively managing the condition. Let’s take a closer look at the different types of narcolepsy and what sets them apart.
Type 1 Narcolepsy
Type 1 Narcolepsy, also known as Narcolepsy with Cataplexy, is the most common form of narcolepsy. It is characterized by excessive daytime sleepiness, sudden muscle weakness or paralysis known as cataplexy, and disruptions to rapid eye movement (REM) sleep.
Excessive Daytime Sleepiness: This symptom is the hallmark of narcolepsy, and individuals with Type 1 Narcolepsy experience it to an extreme degree. They may feel an overwhelming urge to sleep during the day, and may fall asleep involuntarily, even in the midst of an activity.
Cataplexy: This symptom is unique to Type 1 Narcolepsy, and involves sudden muscle weakness or paralysis triggered by strong emotions, such as laughter or surprise. This can cause an individual to collapse or fall asleep suddenly, and can be extremely dangerous if it occurs while operating machinery or driving.
Disruptions to REM Sleep: Individuals with Type 1 Narcolepsy experience disruptions to the natural REM sleep cycle, which can cause vivid dreams, sleep paralysis, and hallucinations, both at the onset of sleep and during daytime naps.
It is important to note that Type 1 Narcolepsy is a chronic condition that typically develops in adolescence or early adulthood and requires lifelong management. If you experience symptoms of Narcolepsy, it is important to consult your physician for a proper diagnosis and appropriate treatment.
Type 2 Narcolepsy
Type 2 Narcolepsy is the less common form of narcolepsy, affecting only 10-20% of narcoleptics. While it shares some symptoms with Type 1 Narcolepsy, the primary difference is the absence of cataplexy – a sudden, temporary loss of muscle control often triggered by strong emotions such as laughter or anger.
Symptoms of Type 2 Narcolepsy
The symptoms of Type 2 Narcolepsy are similar to Type 1, including excessive daytime sleepiness, sudden attacks of sleep, and disrupted nighttime sleep. Other symptoms may include:
- Hypnagogic hallucinations: vivid, dream-like experiences while falling asleep or waking up.
- Sleep paralysis: a temporary inability to move or speak when waking up or falling asleep.
- Automatic behavior: performing routine tasks on autopilot without being fully conscious or aware.
- Insomnia: difficulty falling asleep or staying asleep through the night.
Causes of Type 2 Narcolepsy
Type 2 Narcolepsy is often considered to be idiopathic, meaning that the underlying causes are unknown, although there are certain risk factors and factors that may exacerbate the condition. Some of the risk factors include:
- Genetics: narcolepsy often runs in families, suggesting a genetic predisposition to the disorder.
- Autoimmune disorders: it is thought that Type 2 Narcolepsy may be triggered by an autoimmune disorder, in which the immune system attacks healthy cells in the body.
- Certain infections or illnesses: viral infections such as the flu or strep throat, as well as head injuries or tumors, may increase the risk of developing narcolepsy.
- Poor sleep hygiene: irregular sleep patterns or lack of sleep can exacerbate the symptoms of narcolepsy.
Treatment for Type 2 Narcolepsy
Treatment for Type 2 Narcolepsy typically involves medications and lifestyle changes, similar to those for Type 1 Narcolepsy. Medications may include stimulants to decrease daytime sleepiness, while lifestyle changes may include establishing better sleep hygiene habits and avoiding triggers that can exacerbate symptoms. Certain alternative treatments such as meditation, acupuncture or yoga may also be beneficial.
It is important for individuals with Type 2 Narcolepsy to work closely with a healthcare professional to manage their symptoms and develop an effective treatment plan.
Secondary Narcolepsy
Secondary Narcolepsy is a less common form of narcolepsy, which accounts for less than 10% of all narcolepsy cases. Unlike type 1 and type 2 narcolepsy, secondary narcolepsy occurs as a result of another medical condition or factor. This type of narcolepsy is also known as symptomatic narcolepsy.
Possible Causes of Secondary Narcolepsy
There are several medical conditions or factors that can lead to the development of secondary narcolepsy. Some of these include:
| Possible Causes | Description |
|---|---|
| Brain Injury | Head trauma or injury to the brain may cause damage to the part of the brain responsible for regulating sleep and wake cycles, leading to symptoms of narcolepsy. |
| Neurological Disorders | Conditions such as multiple sclerosis or Parkinson’s disease may damage the brain and contribute to secondary narcolepsy. |
| Infections | Infections such as encephalitis or meningitis can cause inflammation in the brain, resulting in narcolepsy symptoms. |
| Medications or Substance Abuse | Certain medications or substance abuse can lead to changes in the brain and cause narcolepsy-like symptoms. For example, some medications used to treat Parkinson’s disease may cause excessive daytime sleepiness. |
| Psychological Factors | High levels of stress, anxiety or depression may affect the brain and lead to symptoms of narcolepsy. |
Diagnosis of Secondary Narcolepsy
The diagnosis of secondary narcolepsy involves ruling out other medical conditions or factors that may be causing the symptoms. This requires a thorough medical history evaluation, physical examination, and diagnostic tests such as polysomnography and multiple sleep latency tests. In some cases, a brain MRI or CT scan may be required to determine if there is any damage to the brain.
Treatment of Secondary Narcolepsy
The treatment of secondary narcolepsy depends on the underlying cause of the condition. Treating the primary medical condition or factor that is causing the symptoms may alleviate the symptoms of narcolepsy. For example, if the narcolepsy is a result of a brain injury, treating the injury may improve the sleep-wake cycle.
Conclusion
While secondary narcolepsy is rare, it is important to identify and treat the underlying cause to alleviate the symptoms. If you suspect that you or a loved one may have secondary narcolepsy, it is important to seek medical attention and undergo a thorough evaluation to determine the cause of the symptoms.
Diagnosis
One of the biggest challenges in managing narcolepsy is identifying the condition in the first place. Given the wide range of symptoms and the fact that they can be easily mistaken for signs of other issues, diagnosing narcolepsy can be a complicated process. In this section, we’ll explore the various diagnostic tests and criteria that doctors typically rely on to identify narcolepsy. We’ll also offer some guidance on alternative strategies for getting a proper diagnosis if you suspect you may be dealing with this condition.
Diagnostic Tests
Once you suspect that you or someone you know may be experiencing symptoms of narcolepsy, it is important to get a proper diagnosis from a healthcare professional. The diagnosis of narcolepsy involves a variety of diagnostic tests to determine the presence and severity of the condition. Here are some of the most common tests used in diagnosing narcolepsy:
- Nocturnal polysomnogram: This is a test that monitors sleep pattern, brain activity, eye movements, heart rate, and muscle activity while you sleep. This test is usually done overnight, and it helps to rule out other sleep disorders that may have similar symptoms to narcolepsy.
- Multiple sleep latency test: This test involves taking several short daytime naps in a controlled environment after a full night’s sleep. It measures how quickly you fall asleep and if you enter REM sleep during the nap. People with narcolepsy fall asleep very quickly and enter REM sleep early in the nap cycle.
- Hypocretin level test: This test measures the level of hypocretin in the cerebrospinal fluid. People with narcolepsy usually have low levels of hypocretin, which is an important neurotransmitter for regulating wakefulness and sleep.
- Epworth Sleepiness Scale: This is a questionnaire that assesses the likelihood of falling asleep in various situations throughout the day. It is often used as a screening tool for narcolepsy.
It is essential to undergo these tests to provide accurate diagnosis and treatment of narcolepsy. It is best to consult with a healthcare professional about the frequency of these tests and what they entail.
Diagnosis Criteria
When diagnosing narcolepsy, doctors rely on specific criteria to determine if someone has the condition. The criteria include a combination of symptoms and tests, and the diagnosis must be made by a qualified medical professional. Here are the diagnosis criteria that doctors use to identify narcolepsy:
| Criteria | Description |
|---|---|
| Excessive daytime sleepiness | One or more irresistible episodes of need to sleep or daytime lapses into sleep occurring daily over the past three months |
| Cataplexy | Episodes of sudden, bilateral, or generalized muscle weakness, precipitated by strong emotions |
| Hypocretin deficiency | Cerebrospinal fluid hypocretin-1 concentration less than or equal to one-third of values in normal subjects with the cutoff value less than or equal to 110 pg/mL |
| Polysomnogram | Objective documentation of rapid eye movement sleep abnormalities showing at least two sleep-onset REM periods or HLA-DQB1*06:02 positivity, and ruling out other sleep disorders or medical conditions that could explain the clinical features |
It’s important to note that not all people with narcolepsy will have all of these criteria, and alternative diagnostic techniques may be used in some cases. Additionally, it’s essential to rule out other potential causes of sleepiness, such as sleep apnea or depression. If you think you may have narcolepsy, speak to your healthcare provider about your symptoms and concerns.
Treatment

When it comes to managing narcolepsy, several treatment options are available to help control symptoms and improve quality of life. From medications to lifestyle modifications and alternative therapies, finding the right approach can be a daunting task. However, with the guidance of healthcare professionals and support from loved ones, individuals with narcolepsy can lead fulfilling and productive lives. In this section, we will explore various treatment options for narcolepsy and discuss their potential benefits and drawbacks.
Medications
Narcolepsy is a chronic neurological condition that requires the use of medication to treat its symptoms. The goal of medication is to help people with narcolepsy stay awake and alert during the day, as well as to manage other symptoms like cataplexy, sleep paralysis, and hallucinations. There are a few medications available that can help manage these symptoms.
Stimulant Medications:
Stimulant medications are the most common type of medication used to treat narcolepsy. They work by increasing levels of a neurotransmitter called dopamine, which helps to promote wakefulness. Some examples of stimulants used for narcolepsy include modafinil, methylphenidate, and dextroamphetamine. While these medications can be effective at managing symptoms, they do come with side effects like elevated heart rate and blood pressure, insomnia, and anxiety.
Sodium Oxybate:
Sodium oxybate is a medication that’s used to treat both cataplexy and excessive daytime sleepiness in people with narcolepsy. It works by improving the quality of sleep, which in turn can help reduce both symptoms. It’s typically taken in two doses at night, making sodium oxybate an effective option for managing symptoms that occur during sleep like cataplexy and sleep paralysis. However, like any medication, sodium oxybate comes with side effects like nausea, dizziness, and confusion.
Antidepressants:
Some antidepressant medications can be used to manage symptoms of narcolepsy, particularly cataplexy. The most common antidepressants prescribed for cataplexy are selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). While not as effective as other medication options, for some people with mild symptoms, antidepressants may be enough to manage symptoms.
If you have narcolepsy, it’s important to work with a healthcare professional to determine what medication regimen is right for you. While there’s no cure for narcolepsy, medications can help manage symptoms and improve quality of life. It’s important to weigh the benefits of medication against potential side effects and develop a management plan that works best for you.
Lifestyle Changes
Lifestyle changes can play an important role in managing narcolepsy symptoms. Making healthy choices can help you feel more awake and alert during the day. Below are some tips and strategies for making lifestyle changes that can improve your quality of life.
| Tip | Description |
|---|---|
| Follow a regular sleep schedule | Going to bed and waking up at the same time every day can help regulate your sleep-wake cycle. |
| Avoid caffeine and alcohol | Caffeine and alcohol can disrupt your sleep and make you feel more tired during the day. |
| Exercise regularly | Regular exercise can help improve your energy levels and promote better sleep at night. |
| Take short naps | Short naps (less than 30 minutes) can help reduce daytime sleepiness. |
| Avoid large meals and sugar | Large meals and foods high in sugar can make you feel sleepier after eating. |
| Use good sleep hygiene | Create a calming sleep environment by keeping your bedroom cool and dark, and avoiding screens before bedtime. |
| Be mindful of medication side effects | Sleep medications can have side effects that make narcolepsy symptoms worse. Talk to your doctor about any concerns you may have. |
Incorporating these lifestyle changes along with medication and other treatments can help you manage your narcolepsy symptoms and improve your overall quality of life. It’s important to work closely with your healthcare team to find the best treatment plan for you.
Alternative Treatments
Aside from medication and lifestyle changes, there are also alternative treatments that can help manage the symptoms of narcolepsy. These treatments are not backed by scientific evidence and may not work for everyone, but some people have reported success with them. Here are some alternative treatments that you may want to consider:
| Treatment | Description |
|---|---|
| Acupuncture | Acupuncture involves the insertion of needles into specific points on the body to balance energy flow. Some people believe that acupuncture can help improve sleep and reduce fatigue. |
| Meditation | Meditation involves focusing the mind on a specific object, thought, or activity to achieve a mentally clear and emotionally calm state. Some people find that meditation can help reduce stress and improve sleep quality. |
| Yoga | Yoga involves physical postures, breathing techniques, and meditation to improve physical and mental health. Some people find that yoga can help reduce stress and improve sleep quality. |
| Herbal supplements | Some herbs, such as valerian root and chamomile, are believed to have sedative properties that can help improve sleep quality. However, it’s important to talk to your doctor before taking any herbal supplements, as they can interact with medications or cause side effects. |
| Hypnosis | Hypnosis involves entering a state of deep relaxation and concentration to achieve a heightened level of suggestibility. Some people find that hypnosis can help improve sleep quality and reduce fatigue. |
It’s important to note that these alternative treatments should be used in conjunction with medication and lifestyle changes, not as a replacement for them. If you’re interested in trying any of these treatments, be sure to talk to your doctor first to make sure they’re safe for you and won’t interfere with your other treatments.
Living with Narcolepsy

Adjusting to life with narcolepsy can be a challenging experience. Individuals with narcolepsy may struggle with managing their symptoms and adapting to the impact narcolepsy can have on their daily routine. Coping strategies, support groups and proper treatment can make living with narcolepsy more manageable. Let’s explore some ways individuals with narcolepsy can live a fulfilling and healthy life.
Managing Symptoms
One of the main challenges of living with narcolepsy is managing the symptoms. There are several strategies that can help individuals with narcolepsy cope with the symptoms and improve their overall quality of life. Here are some tips for managing narcolepsy symptoms:
- Stick to a regular sleep schedule: Maintaining a consistent sleep schedule can help regulate the sleep-wake cycle and reduce daytime sleepiness. Establish a routine and try to go to bed and wake up at the same time every day, even on weekends.
- Take short naps: Taking brief, 20-30 minute naps throughout the day can help alleviate daytime sleepiness and improve alertness. However, avoid napping too close to bedtime, as this can interfere with nighttime sleep.
- Avoid caffeine and alcohol: Both caffeine and alcohol can disrupt sleep and make it more difficult to fall and stay asleep. Avoid consuming these substances, especially in the evening.
- Exercise regularly: Regular exercise can help reduce fatigue and improve overall health. However, avoid exercising too close to bedtime, as this can interfere with nighttime sleep.
- Take prescribed medications as directed: There are several medications available to help manage the symptoms of narcolepsy. It is important to take these medications exactly as prescribed by a healthcare provider.
- Avoid driving or operating heavy machinery: Individuals with narcolepsy may experience sudden bouts of sleepiness or cataplexy, which can be dangerous when driving or operating heavy machinery. It is important to avoid these activities if experiencing any symptoms.
- Reduce stress: Stress can exacerbate the symptoms of narcolepsy. Practicing relaxation techniques, such as deep breathing or yoga, can help reduce stress and improve overall well-being.
By incorporating these strategies into daily life, individuals with narcolepsy can better manage their symptoms and improve their quality of life. However, it is important to work with a healthcare provider to develop an individualized treatment plan and constantly reevaluate the effectiveness of any strategies or medications being used.
Support Groups
Support groups can be a valuable resource for individuals with narcolepsy. These groups offer a supportive and understanding environment for those affected by the disorder. Support groups can provide a sense of community that can make a big difference in coping with the challenges of narcolepsy. Members of these groups can share their experiences, offer insights into management techniques, and provide emotional support.
There are numerous support groups both online and in-person that cater specifically to those with narcolepsy. These groups can offer a wealth of information on the latest treatments and coping strategies. They can also provide a platform for members to voice their concerns and connect with others in similar situations.
Many support groups offer regular meetings, where members can come together to meet new people and discuss their experiences. These meetings may be in-person or online, allowing members to connect from anywhere in the world. Some support groups offer workshops, educational resources, and social events, all geared towards helping members manage their narcolepsy.
It is important for those with narcolepsy to know they are not alone. Support groups offer a space where individuals can feel understood and supported. They can be a valuable tool in helping members manage the impact of narcolepsy on their lives. Whether it is finding new coping strategies, connecting with others who share similar experiences, or simply having a supportive and understanding community, support groups can make a big difference for those affected by narcolepsy.
Some popular narcolepsy support groups include:
- Narcolepsy Network
- A.W.A.K.E. (Alert, Well, and Keeping Energetic) Network
- The Hypersomnia Foundation
These groups provide a range of resources and support for individuals with narcolepsy, including meetings, forums, and educational resources. By becoming part of a support group, individuals with narcolepsy can develop new skills and strategies to help them manage their symptoms and improve their quality of life.
Coping Strategies
Living with Narcolepsy can be challenging, but there are strategies you can use to manage the symptoms and improve your quality of life. Here are some coping strategies that can help:
- Create a sleep-friendly environment: Make sure your bedroom is cool, dark, and quiet. Use comfortable bedding and invest in a supportive pillow.
- Stick to a regular sleep schedule: Go to bed and wake up at the same time every day, even on weekends. This can help regulate your body clock and improve sleep quality.
- Take short naps: If you feel tired during the day, taking a short nap (less than 30 minutes) can help you feel more alert. Avoid napping for too long or too late in the day.
- Avoid caffeine and alcohol: These substances can interfere with sleep quality and exacerbate symptoms of Narcolepsy.
- Stay active: Regular exercise can help improve sleep quality and reduce fatigue. Talk to your doctor about safe and appropriate exercises for you.
- Practice stress-management techniques: Stress can worsen symptoms of Narcolepsy, so it’s important to find ways to manage stress. Try techniques like deep breathing, meditation, or yoga.
- Stay hydrated: Dehydration can worsen symptoms of Narcolepsy, so make sure you’re drinking enough water throughout the day.
Remember, coping with Narcolepsy is a journey, and it’s different for everyone. What works for one person may not work for another. Be patient with yourself, and don’t hesitate to seek support from loved ones or a mental health professional.
Complications and Risks
As with any medical condition, narcolepsy comes with its own set of complications and risks. These can range from physical dangers to emotional and social challenges that impact a person’s quality of life. It’s important to understand these potential complications and risks in order to manage narcolepsy effectively and live a fulfilling life. Let’s take a look at some of the specific concerns associated with this sleep disorder.
Dangers of Untreated Narcolepsy
Untreated Narcolepsy can lead to several adverse effects on an individual’s physical and mental health. Below are some of the dangers of untreated Narcolepsy:
| Excessive Daytime Sleepiness (EDS): | People with Narcolepsy experience an uncontrollable urge to sleep during the day, which can interfere with the ability to carry out daily activities such as driving, working, or studying. Untreated EDS can increase the risk of accidents and injuries. |
| Cataplexy: | Cataplexy is a sudden loss of muscle tone triggered by intense emotions such as laughter, anger, or surprise. It can cause the person to fall down or be unable to move for a brief period. Untreated Cataplexy can lead to social isolation, depression, and anxiety. |
| Hallucinations: | Narcolepsy can cause vivid and often frightening experiences during sleep and wakefulness. These hallucinations can be distressing and affect an individual’s mental well-being. Untreated Narcolepsy can lead to severe depression and anxiety. |
| Sleep-Related Disorders: | Untreated Narcolepsy can increase the risk of other sleep-related disorders such as sleep apnea, insomnia, and restless legs syndrome. These conditions can further affect an individual’s quality of life and lead to long-term health problems. |
| Obesity: | Studies have shown that people with Narcolepsy are at a higher risk of developing obesity due to the disruption of sleep-wake cycles, leading to hormonal changes that affect metabolism. Untreated Narcolepsy can result in weight gain and associated health issues such as diabetes and heart disease. |
It is important to seek medical help if you suspect that you or someone you know may be suffering from Narcolepsy. Treatment can help manage the symptoms and prevent the potential dangers associated with untreated Narcolepsy.
Safety Precautions
To ensure safety and minimize risks associated with narcolepsy, there are several measures that individuals can take. These safety precautions include:
| Driving | Individuals with narcolepsy should avoid driving until their symptoms are well-managed with treatment. Driving without proper treatment can be dangerous due to sudden loss of muscle control, hallucinations, and falling asleep at the wheel. |
| Working at Heights | Individuals with cataplexy episodes should avoid working at heights or on rooftops to avoid the risk of serious injury if they experience sudden muscle weakness and collapse. |
| Swimming | It is important to ensure that lifeguards or other individuals are aware of the individual’s narcolepsy diagnosis and symptoms, particularly if they experience cataplexy, to avoid any potential incidents while swimming or participating in water activities. |
| Machinery and Equipment | Individuals with narcolepsy should avoid working with heavy machinery or equipment that could potentially lead to injuries if they fall asleep or experience sudden muscle weakness. |
| Medic Alert Bracelet | Wearing a medical alert bracelet can be helpful to first responders or medical professionals in the event of an emergency, particularly if the individual is incapacitated and unable to communicate their condition. |
By taking these safety precautions, individuals with narcolepsy can minimize the risks associated with their symptoms and live a safer, more manageable life. However, it is important to keep in mind that proper treatment and symptom management are the most effective ways to reduce the risk of accidents and injuries associated with narcolepsy.
Conclusion
In conclusion, narcolepsy is a chronic sleep disorder that affects a significant number of individuals worldwide. It can be a highly debilitating condition that can severely impact an individual’s quality of life. The disorder is characterized by excessive daytime sleepiness, sudden muscle weakness or paralysis, and hallucinations.
While the exact causes of narcolepsy are still not completely understood, researchers believe that it may be linked to genetic factors, as well as abnormalities in certain brain chemicals such as hypocretin.
There are different types of narcolepsy, which are determined by the severity and duration of symptoms. These include Type 1, Type 2, and Secondary Narcolepsy. The treatments for narcolepsy include medications, lifestyle changes, and alternative treatments.
People living with narcolepsy may face numerous complications and risks, including the dangers of untreated narcolepsy and a number of safety precautions that must be taken. By managing symptoms effectively and having access to support groups, individuals with this condition can lead fulfilling lives.
While there is no cure for narcolepsy, research is ongoing and advancements are being made in understanding and managing this condition. So if you or a loved one are experiencing symptoms, it’s important to seek the help of a healthcare professional who can guide you in managing the condition effectively.
Frequently Asked Questions
What are the common symptoms of narcolepsy?
The common symptoms of narcolepsy include excessive daytime sleepiness, sudden loss of muscle tone, hallucinations, sleep paralysis, and disrupted nighttime sleep.
What causes narcolepsy?
The exact cause of narcolepsy is unclear, but it is believed to be related to a deficiency of hypocretin, a neurotransmitter that regulates sleep-wake cycles. This deficiency may be due to genetic or environmental factors, or a combination of both.
What are the types of narcolepsy?
The types of narcolepsy include type 1 narcolepsy, type 2 narcolepsy, and secondary narcolepsy.
What is type 1 narcolepsy?
Type 1 narcolepsy is characterized by excessive daytime sleepiness, sudden loss of muscle tone, hallucinations, and sleep paralysis. It is also known as narcolepsy with cataplexy.
What is type 2 narcolepsy?
Type 2 narcolepsy is characterized by excessive daytime sleepiness, but without cataplexy.
What is secondary narcolepsy?
Secondary narcolepsy is caused by an underlying condition or injury, such as a brain injury, infection, or hormone imbalance.
How is narcolepsy diagnosed?
Narcolepsy is diagnosed through a combination of diagnostic tests and meeting specific criteria, such as frequent daytime sleep attacks and cataplexy.
What medications are used to treat narcolepsy?
Medications used to treat narcolepsy include stimulants to promote wakefulness, sodium oxybate to improve nighttime sleep, and antidepressants to manage cataplexy and other symptoms.
Can lifestyle changes help manage narcolepsy symptoms?
Yes, lifestyle changes such as maintaining a regular sleep schedule, avoiding caffeine and alcohol, and taking short naps during the day can help manage narcolepsy symptoms.
What are some coping strategies for living with narcolepsy?
Coping strategies for living with narcolepsy include educating family and friends about the condition, practicing good sleep hygiene, and developing a support network.