As humans, we spend approximately one-third of our lives sleeping. During this time, our bodies undergo various sleep cycles, including the rapid eye movement (REM) stage. For most people, this stage is characterized by paralysis of the muscles, which prevents them from physically acting out the vivid dreams that occur. However, some people experience a condition known as REM Sleep Behavior Disorder (RBD), in which this paralysis does not occur, leading to potentially harmful movements during sleep. The implications of untreated RBD can be serious, from injuries to oneself or sleeping partners to an increased risk of developing Parkinson’s disease or dementia. In this article, we will explore the various complications of untreated RBD, as well as the causes, symptoms, diagnosis, and treatment options available for those who suffer from this condition.
What is REM Sleep Behavior Disorder

Sleep is essential for our physical and mental health, but when it is disrupted, it can lead to a variety of conditions. One of the lesser-known sleep disorders is REM Sleep Behavior Disorder (RBD). RBD is a condition where a person lacks the usual paralysis that occurs during rapid eye movement (REM) sleep, resulting in the person physically acting out their dreams during sleep. This can lead to various complications if left untreated. Let’s dive in and learn more about RBD, including its definition, prevalence, causes, and symptoms.
Definition of REM Sleep Behavior Disorder
REM Sleep Behavior Disorder, also known as RBD, is a type of sleep disorder that causes people to act out their dreams, often violently. It is a condition that occurs during the rapid eye movement (REM) stage of sleep, which is the stage during which people experience their most vivid dreams.
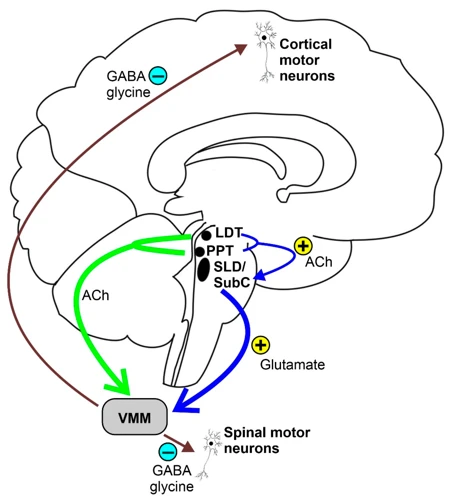
This disorder is characterized by the loss of the normal muscle paralysis that occurs during REM sleep, which allows people to act out their dreams. People with RBD may scream, shout, kick, punch, or even jump out of bed, which can lead to injuries to themselves or their sleeping partners.
| Key Features | Description |
|---|---|
| REM Stage of Sleep | RBD occurs during the rapid eye movement (REM) stage of sleep. |
| Loss of Muscle Paralysis | RBD is characterized by the loss of the normal muscle paralysis that occurs during REM sleep, which allows people to act out their dreams. |
| Violent Movements | People with RBD may scream, shout, kick, punch, or even jump out of bed, which can lead to injuries to themselves or their sleeping partners. |
RBD can be a very distressing condition for both the person experiencing it and their partner or other family members who may be sleeping nearby. It can also have serious consequences if left untreated, which is why it is important to seek medical attention if you believe you may be suffering from RBD.
Prevalence of REM Sleep Behavior Disorder
According to various studies, the prevalence of REM Sleep Behavior Disorder (RBD) varies across different populations and age groups. Here are some key findings:
- In the general population, the prevalence of RBD is estimated to be between 0.5% and 1%.
- RBD is more common in men than women, with a male-to-female ratio of approximately 2:1.
- The incidence of RBD increases with age, with the highest rates observed among people over 60 years old.
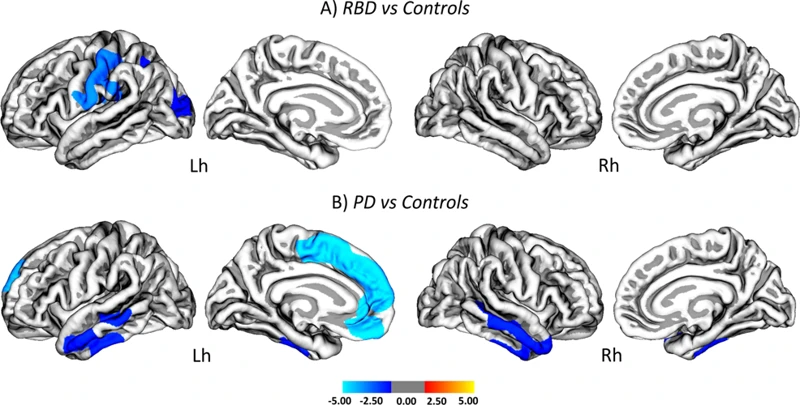
- RBD has also been associated with certain neurological conditions, including Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy.
- In patients with Parkinson’s disease, the prevalence of RBD has been reported to be as high as 50%.
- Individuals with RBD have been found to be more likely to have a history of head injury compared to those without RBD.
These findings suggest that RBD is a relatively rare condition in the general population, but becomes more prevalent with age and in certain neurological populations. Men are more likely to be affected than women, and RBD may be associated with a history of head injury. Further research is needed to better understand the causes of RBD and its relationship to other health conditions.
Causes of REM Sleep Behavior Disorder
REM Sleep Behavior Disorder (RBD) is a sleep disorder that makes people act out their dreams while they’re in the REM stage of sleep. The exact causes of RBD are not fully understood, but research indicates that various factors such as age, gender, genetics, and certain medical conditions might contribute to the development of this condition.
Below are some of the possible causes of RBD:
| Aging | REM sleep behavior disorder is more common among older adults, and research suggests that it might be linked to age-related changes in the brain. |
| Gender | Men are twice as likely as women to develop RBD, and the reason for this is not fully understood. |
| Genetics | Studies have found that some cases of RBD might have a genetic component, with the disorder running in families. |
| Medical conditions | RBD has been associated with certain medical conditions such as Parkinson’s disease, multiple system atrophy, and narcolepsy. In some cases, RBD might be an early sign of these conditions. |
| Medications | Certain medications, such as antidepressants, might increase the risk of developing RBD. Additionally, the withdrawal from certain medications can also trigger RBD symptoms. |
It is important to note that not everyone with these risk factors will develop RBD, and some people might develop RBD without having any of these risk factors. More research is needed to fully understand the causes of RBD and how best to prevent and treat it.
Symptoms of REM Sleep Behavior Disorder
REM Sleep Behavior Disorder is characterized by disruptive and violent movements during the REM phase of sleep. Some of the common symptoms associated with this sleep disorder are:
- Acting out dreams: This is the main symptom of REM Sleep Behavior Disorder, where the individual physically acts out their dreams while sleeping. These actions can be mild, such as talking or sitting up in bed, or can be violent like punching, kicking, or jumping out of bed.
- Loud noises during sleep: The individual may make loud noises due to shouting, screaming, or other vocalizations while experiencing vivid dreams.
- Injury to self or sleeping partner: As a result of the violent movements during sleep, the individual may injure themselves or their sleeping partner accidentally.
- Frequent awakenings: The individual may frequently wake up, either due to the movements or from the vivid dreams, and have difficulty falling back to sleep.
- Feeling tired during the day: Due to insufficient sleep and frequent awakenings, the individual may feel excessively tired and sleepy during the day.
- Memory problems: The individual may have problems with memory and forgetfulness, which can affect their daily functioning.
- An increase in anxiety or depression: The individual may experience an increase in anxiety or depression due to the poor quality of sleep and frequent disruptions.
It is important to note that not all individuals experience all of these symptoms, and severity can vary greatly among cases. If you or someone you know is experiencing any of these symptoms, it is important to seek medical advice to determine if REM Sleep Behavior Disorder is the underlying cause.
Complications of Untreated REM Sleep Behavior Disorder
Untreated REM Sleep Behavior Disorder can lead to a variety of serious complications that impact both the affected individual and their sleeping partner. These complications range from physical injury to declining quality of life, and may even increase the risk of developing more severe neurological conditions such as Parkinson’s disease and dementia. It is crucial to understand the potential consequences of not addressing REM Sleep Behavior Disorder in order to seek timely treatment and prevent further complications.
Injury to Self and Sleeping Partner
REM Sleep Behavior Disorder can pose a risk of injury not only to oneself but also to sleeping partners. People with this disorder often experience vivid and intense dreams that cause them to act out physically while asleep. These can range from simple movements like talking or flailing of the arms to more complex behaviors like jumping out of bed or even hitting or kicking their sleeping partner.
This can lead to:
| 1 | Injuries to oneself from falling out of bed or striking furniture or objects in the room during sleep |
| 2 | Bruising, concussion or fractures for the sleeping partner who may be on the receiving end of the physical hostilities |
Not only can this cause physical harm, but it can also lead to emotional distress and strain on the relationship between partners. The consequences of such injuries can be severe, especially if the person with REM Sleep Behavior Disorder is not properly diagnosed or treated, resulting in a potentially dangerous situation.
It is essential to take necessary precautions to prevent injuries from occurring. Sleeping in separate beds or bedrooms can be a viable solution. Bed rails or padding the floor around the bed can also offer a degree of protection. Additionally, creating a safe sleeping environment by removing any objects that could cause harm or injury can help reduce the risk of injury. Seeking medical attention and proper treatment can help alleviate the symptoms, thereby minimizing the chances of harm to oneself or their sleeping partner.
Declining Quality of Life
REM Sleep Behavior Disorder, if left untreated, can lead to a marked decline in the quality of life of the patients. This disorder affects the sleep cycle of the body and, as a result, impacts several physiological and psychological functions. Here are some of the ways in which untreated REM Sleep Behavior Disorder can affect an individual’s quality of life:
| Effect of Untreated RBD | Description |
|---|---|
| Excessive Daytime Sleepiness | Patients with RBD often struggle with excessive daytime sleepiness, which can impact their ability to function well during the day. They may feel lethargic and/or experience micro-sleep during the day, which can increase the risk of accidents. |
| Fatigue and Low Energy Levels | RBD can affect the quality of sleep that patients receive, resulting in low energy levels and persistent fatigue. This can leave them feeling depleted and unable to enjoy everyday activities. |
| Depression and Anxiety | Patients with RBD may also suffer from mood disturbances, such as depression and anxiety. Sleep deprivation can significantly impact the mood-regulation system of the body, causing emotional distress. |
| Difficulty in Performing Daily Tasks | As RBD affects the sleep pattern, patients may find it difficult to perform daily tasks with precision and ease. A decline in cognitive function along with poor concentration and attention can make it challenging to perform even simple tasks. |
| Reduced Social Interaction | Patients with RBD may also experience social isolation due to their inability to sleep well at night. This can lead to a decrease in social activities and can result in further psychological issues. |
These are just a few of the ways in which untreated REM Sleep Behavior Disorder can affect a person’s quality of life. Seeking medical assistance and following the recommended treatment plan can significantly improve the patient’s condition, leading to a better quality of life.
Increased Risk of Parkinson’s Disease and Dementia
According to research, individuals who suffer from untreated REM Sleep Behavior Disorder are at an increased risk of developing two serious neurological disorders: Parkinson’s disease and dementia.
Studies have shown that individuals with REM Sleep Behavior Disorder have a significantly higher chance of developing Parkinson’s disease later in life compared to those who don’t suffer from the disorder. In fact, one study found that up to 75% of individuals with REM Sleep Behavior Disorder will eventually develop Parkinson’s disease or a similar condition.
Additionally, several studies have shown that individuals with REM Sleep Behavior Disorder are at a significantly increased risk of developing dementia. During REM sleep, the brain consolidates memories and flushes out toxins, and when REM Sleep Behavior Disorder occurs, the brain is not able to carry out these functions properly, leading to an increased risk of dementia.
It is imperative that individuals with REM Sleep Behavior Disorder seek treatment, as this can help reduce the risk of developing Parkinson’s disease and dementia. Patients who are already suffering from these conditions and have REM Sleep Behavior Disorder should seek treatment for both conditions simultaneously, as this can help improve overall outcomes.
Diagnosis of REM Sleep Behavior Disorder
Determining if one has REM sleep behavior disorder can be a complex process that involves various types of medical examinations and testing. Physicians will need to take a detailed medical history, perform a physical examination, and conduct a number of laboratory tests to confirm whether or not REM sleep behavior disorder is present. In this section of the article, we will explore the diagnostic methods that healthcare professionals may use to diagnose REM sleep behavior disorder and gain insight into the specific tests that patients might expect to undergo.
Medical History and Physical Examination
The first step to diagnosing REM Sleep Behavior Disorder (RBD) is taking a thorough medical history and conducting a physical examination. This is crucial because RBD can often be a symptom of other underlying conditions such as Parkinson’s disease, multiple system atrophy, or Lewy body dementia. The table below outlines key factors that doctors may consider during the medical history and physical examination process:
| Medical History | Physical Examination |
|---|---|
| Medical conditions: doctors will ask about current medical conditions and any medications being taken. | Neurological exam: this may include tests of strength, reflexes, coordination, and sensation. |
| Personal history: doctors may ask about alcohol or drug use, changes in mood or behavior, or recent head injuries. | Fall risk assessment: doctors may assess balance and gait to determine fall risk during sleepwalking episodes. |
| Family history: doctors may ask about any family history of neurological disorders. | Sleep disturbance evaluation: doctors may ask about symptoms of other sleep disturbances such as sleep apnea, insomnia, or restless leg syndrome. |
During the physical examination, doctors may look for signs of other neurological disorders or injuries that could be contributing to the symptoms. They may also assess for any physical injuries sustained from incidents related to RBD, such as bruises or cuts. A thorough medical history and physical examination can help doctors identify potential underlying causes of RBD and determine the best course of treatment.
Nocturnal Polysomnography and Video Polysomnography
Nocturnal Polysomnography and Video Polysomnography: These are the most reliable and accurate diagnostic tools for REM sleep behavior disorder. They involve an overnight stay at a sleep center where the patient’s brain waves, breathing, heart rate, oxygen levels, and muscle activity are recorded and monitored.
- During nocturnal polysomnography, electrodes are attached to the patient’s scalp, face, chest, and legs to measure brain activity, eye movements, muscle tone, heart rate, and breathing.
- Video polysomnography is similar to nocturnal polysomnography, but it also includes video recording of the patient’s movements and behaviors during sleep. This allows for direct observation of any abnormal behaviors, such as kicking, punching, or flailing.
These tests can help to distinguish REM sleep behavior disorder from other sleep disorders, such as sleepwalking or night terrors. They can also help to identify any underlying conditions that may be contributing to the disorder, such as Parkinson’s disease.
However, it’s important to note that these tests are not always necessary for diagnosis. In some cases, a medical history and physical examination may be enough to diagnose REM sleep behavior disorder, especially if the symptoms are clear and consistent.
Actigraphy
Actigraphy is a non-invasive method to monitor activity and sleep-wake patterns in individuals. It involves the use of a small device, called an actigraph, that is worn on the wrist like a watch. The actigraph measures movement and activity levels, which can be used to estimate sleep duration and quality.
Advantages of Actigraphy
Actigraphy has several advantages over other methods of monitoring sleep. It is non-invasive and does not require electrodes or wires to be attached to the body, making it more comfortable and less obtrusive for individuals. It can also be used in the individual’s natural sleeping environment, unlike polysomnography, which is typically conducted in a sleep laboratory. This allows for a more accurate representation of the individual’s sleep-wake patterns in their normal routine.
How Actigraphy Works
The actigraph measures movement and activity levels using a small accelerometer. The accelerometer detects changes in movement and converts them into electrical signals, which are then recorded by the device. These recordings can be used to estimate the individual’s level of activity and sleep-wake patterns.
Interpreting Actigraphy Results
The data collected by the actigraph can provide valuable insights into an individual’s sleep-wake patterns. Sleep onset and offset can be estimated by analyzing periods of prolonged inactivity or low activity levels. The data can also reveal the total amount of sleep obtained, as well as the number and duration of awakenings throughout the night.
Actigraphy can help diagnose REM Sleep Behavior Disorder by monitoring the individual’s movements during sleep. It can also be used to track the efficacy of treatment interventions.
Limitations of Actigraphy
While actigraphy is a useful tool for monitoring sleep-wake patterns, it has some limitations. It cannot distinguish between different stages of sleep, such as REM and non-REM sleep. It also cannot detect sleep disorders, such as sleep apnea or restless leg syndrome, that require other methods of diagnosis. Additionally, the accuracy of the data collected by the actigraph can be affected by factors such as the individual’s age, sex, and level of physical activity.
Actigraphy is a valuable tool for monitoring sleep-wake patterns in individuals. While it has some limitations, it can provide valuable insights into an individual’s sleep habits and help diagnose and manage sleep disorders.
Treatment of REM Sleep Behavior Disorder

As REM Sleep Behavior Disorder can lead to a range of potential complications, it is crucial to seek appropriate treatment if you suspect you or someone you know may be experiencing it. Treatment options can help manage symptoms and reduce the risk of harm to oneself or others sleeping nearby. Let’s explore some of the options available for treating REM Sleep Behavior Disorder.
Clonazepam (Klonopin)
One of the most common treatments for REM Sleep Behavior Disorder is Clonazepam, which is also known as Klonopin. Clonazepam belongs to a class of drugs called benzodiazepines, which work by increasing the effects of a neurotransmitter called gamma-aminobutyric acid (GABA) in the brain. This helps to reduce anxiety, muscle spasms, and seizures. Clonazepam is available in tablet form and is usually taken before bedtime.
How Clonazepam Helps with REM Sleep Behavior Disorder
Clonazepam is effective in reducing the symptoms of REM Sleep Behavior Disorder by suppressing the muscle activity during Rapid Eye Movement (REM) sleep. This medication can help reduce or eliminate the physical movements and vocalizations associated with the disorder. It can also help to prevent injury to the patient or their sleeping partner.
Side Effects of Clonazepam
While Clonazepam can be effective in treating REM Sleep Behavior Disorder, it is important to be aware of the potential side effects. Some common side effects of Clonazepam include drowsiness, dizziness, poor coordination, and difficulty thinking or remembering. In some cases, Clonazepam may also cause more serious side effects, such as confusion, depression, and suicidal thoughts.
Precautions when taking Clonazepam
Before taking Clonazepam, it is important to talk to a healthcare provider to determine if it is a safe and appropriate treatment option. Individuals who are allergic to benzodiazepines or who have a history of liver disease or glaucoma may not be able to take Clonazepam. Pregnant or breastfeeding women should also avoid this medication.
| Advantages | Disadvantages |
|---|---|
|
|
Conclusion
Clonazepam is one of several medication options available for individuals with REM Sleep Behavior Disorder. While it can be effective in reducing the symptoms of the disorder, it is important to be aware of the potential side effects and precautions that come with taking this medication. Before beginning any course of treatment, individuals should talk to their healthcare provider to determine if Clonazepam is the right choice for their specific needs.
Melatonin
Melatonin is a hormone that plays a crucial role in regulating sleep-wake cycles. It is naturally produced by the pineal gland in the brain in response to the amount of light in our environment. Studies have shown that melatonin supplementation can effectively treat REM sleep behavior disorder.
Melatonin supplements are available over-the-counter in doses ranging from 1 mg to 10 mg. It is important to note, however, that melatonin is not regulated by the FDA and may vary in purity and potency.
When taking melatonin for REM sleep behavior disorder, it is recommended to start with a lower dose and gradually increase as needed. Taking melatonin 1-2 hours before bedtime can help regulate the sleep-wake cycle and decrease REM sleep behavioral events.
While melatonin is generally considered safe, it can cause side effects such as dizziness, headache, and nausea. It can also interact with certain medications such as blood thinners and antidepressants, so it is important to consult with a healthcare provider before starting melatonin supplementation.
Melatonin supplementation is a viable option for treating REM sleep behavior disorder and improving sleep quality. However, individuals should use caution when choosing a melatonin supplement and follow dosing guidelines closely.
Antidepressants
Antidepressants are medications that can be used to treat REM Sleep Behavior Disorder (RBD) by reducing the intensity of muscle movement during sleep. They work by altering the levels of neurotransmitters in the brain, such as serotonin and norepinephrine, which play a role in regulating sleep patterns.
There are several classes of antidepressants, each with their own unique mechanism of action. Some of the commonly prescribed antidepressants for RBD include selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), and serotonin-norepinephrine reuptake inhibitors (SNRIs).
SSRIs are the most commonly prescribed antidepressants for RBD. They work by blocking the reuptake of serotonin in the brain, which increases its availability and enhances its effects on the body. Examples of SSRIs include:
| Drug Name | Brand Name |
| Fluoxetine | Prozac |
| Paroxetine | Paxil |
| Sertraline | Zoloft |
TCAs are another class of antidepressants that can be used to treat RBD. They work by blocking the reuptake of both serotonin and norepinephrine in the brain, which increases their availability and enhances their effects on the body. Examples of TCAs include:
| Drug Name | Brand Name |
| Amitriptyline | Elavil |
| Imipramine | Tofranil |
| Clomipramine | Anafranil |
SNRIs are a newer class of antidepressants that can also be used to treat RBD. They work by blocking the reuptake of both serotonin and norepinephrine in the brain, similar to TCAs. However, they have a more specific mechanism of action and are generally better tolerated than TCAs. Examples of SNRIs include:
| Drug Name | Brand Name |
| Venlafaxine | Effexor |
| Duloxetine | Cymbalta |
It is important to note that antidepressants may not be effective for everyone with RBD, and they can have side effects such as drowsiness, nausea, and sexual dysfunction. They should only be taken under the guidance of a healthcare professional.
Lifestyle Changes for REM Sleep Behavior Disorder
Making certain lifestyle changes and practicing good sleep habits can be very helpful for people with REM Sleep Behavior Disorder (RBD). These changes help promote better sleep and reduce the frequency and severity of RBD episodes. By avoiding certain triggers, maintaining a regular sleep routine, and improving sleep hygiene, people with RBD can significantly improve their quality of sleep and overall well-being. In this section, we will discuss some practical lifestyle changes that can be helpful for people with RBD.
Avoiding Triggers
One of the key lifestyle changes that can help manage REM sleep behavior disorder is avoiding triggers that can worsen the symptoms. Below are some examples of triggers that should be avoided:
- Stress: Stress can exacerbate the symptoms of REM sleep behavior disorder, so it is important to identify and eliminate sources of stress in your life as much as possible. This can include practicing relaxation techniques such as yoga or meditation, or seeking the help of a therapist to learn coping mechanisms.
- Alcohol: Alcohol consumption can increase the likelihood of acting out dreams during sleep, so it is important to limit or avoid alcohol intake, particularly in the evening.
- Caffeine: Caffeine can interfere with sleep, so it is important to limit or avoid caffeine intake, particularly in the evening.
- Smoking: Nicotine is a stimulant that can interfere with sleep, so it is important to quit smoking or limit nicotine intake.
- Heavy meals: Eating a heavy meal or snacking before bed can trigger symptoms of REM sleep behavior disorder, so it is important to avoid heavy meals or snacks in the evening.
- Irregular sleep patterns: Irregular sleep patterns can disrupt the body’s natural sleep-wake cycle and worsen symptoms of REM sleep behavior disorder, so it is important to maintain a regular sleep schedule as much as possible.
By avoiding these triggers, individuals with REM sleep behavior disorder can decrease the frequency and intensity of their symptoms, and improve overall sleep quality.
Maintaining a Sleep Routine
Maintaining a consistent sleep routine is crucial for managing REM Sleep Behavior Disorder. The following table outlines some tips for establishing and maintaining a regular sleep routine:
| Tip | Description |
|---|---|
| Set a bedtime and wake-up time | Go to bed and wake up at the same time every day, even on weekends. |
| Avoid naps | Avoid taking naps during the day as this can disrupt nighttime sleep. |
| Avoid caffeine and alcohol | Avoid consuming caffeine and alcohol as they can disrupt sleep and worsen REM Sleep Behavior Disorder symptoms. |
| Create a relaxing bedtime routine | Develop a relaxing bedtime routine, such as taking a warm bath or reading a book. |
| Create a sleep-conducive environment | Make sure your bedroom is cool, quiet, and dark to promote a good night’s sleep. |
| Avoid stimulating activities | Avoid stimulating activities before bedtime, such as watching TV or using electronic devices. |
| Exercise regularly | Regular exercise can help regulate sleep patterns, but avoid exercising too close to bedtime. |
By following the tips in the table, individuals with REM Sleep Behavior Disorder can establish and maintain a consistent sleep routine, which can improve the quality of their sleep and reduce the frequency and severity of their symptoms.
Improving Sleep Hygiene
It’s essential to have good sleep hygiene practices to manage REM Sleep Behavior Disorder. Here are a few tips to improve sleep hygiene:
| Tip | Description |
|---|---|
| Avoid Stimulating Activities Before Bed | Stimulating activities like watching TV or using electronic devices should be avoided before bed as they can increase anxiety and make it challenging to fall asleep. |
| Limit Caffeine and Alcohol Intake | Caffeinated or alcoholic drinks should be avoided before bedtime as they can disrupt sleep patterns. |
| Make the Sleeping Environment Comfortable | Ensure that the sleeping environment is comfortable and conducive to sleep. The room should be dark, cool, and quiet. A comfortable mattress and pillow are necessary for a good night’s rest. |
| Stick to a Sleep Schedule | Going to bed and waking up at the same time every day will help regulate the body’s sleep-wake cycle. |
| Relaxation Techniques | Relaxation techniques like meditation, deep breathing, and progressive muscle relaxation can help reduce anxiety and promote better sleep. |
By Implementing these tips, people with REM Sleep Behavior Disorder can minimize the risk of injury to themselves or their partners and improve their quality of life.
Conclusion
In conclusion, it is important to recognize the potential dangers and consequences of untreated REM Sleep Behavior Disorder. The disorder can lead to injury to oneself or a sleeping partner, as well as a declining quality of life. Furthermore, studies have shown that individuals with untreated REM Sleep Behavior Disorder have an increased risk of developing Parkinson’s Disease and dementia.
Early diagnosis and treatment can help manage symptoms and reduce the risk of complications. A medical history and physical examination, nocturnal polysomnography and video polysomnography, and actigraphy are among the diagnostic tools available for REM Sleep Behavior Disorder.
Treatment options include medications such as Clonazepam or Melatonin, as well as lifestyle changes such as avoiding triggers and maintaining healthy sleep hygiene. In addition, support from healthcare professionals, family, and friends can also play an important role in managing the disorder and improving overall quality of life.
It is crucial for those experiencing symptoms to seek medical attention and to educate themselves on the potential risks of leaving REM Sleep Behavior Disorder untreated. By taking necessary steps towards diagnosis and treatment, individuals can improve their overall health and well-being.
Frequently Asked Questions
Can REM Sleep Behavior Disorder be mistaken for other sleep disorders?
Yes, it can be misdiagnosed as insomnia, nightmares or sleep apnea because the physical movements occurring during REM sleep are not always noticed by the person experiencing them.
Does everyone with REM Sleep Behavior Disorder need treatment?
It depends on the severity of symptoms and risk of injury to self or sleeping partners. Mild cases may not need treatment, whereas severe cases should be treated to avoid complications.
Can medication use cause REM Sleep Behavior Disorder?
Yes, certain antidepressants and other medications can cause or worsen REM Sleep Behavior Disorder. It is important to discuss all medications with a healthcare provider.
Is REM Sleep Behavior Disorder hereditary?
There is some evidence to suggest that it may be, especially in cases where there is a family history of Parkinson’s disease, as the two conditions can be connected.
Is there a cure for REM Sleep Behavior Disorder?
There is no known cure for REM Sleep Behavior Disorder, but it can be managed successfully with medication and lifestyle changes.
What is the difference between REM Sleep Behavior Disorder and sleepwalking?
The main difference is that sleepwalking occurs during non-REM sleep, whereas REM Sleep Behavior Disorder occurs during REM sleep. Additionally, sleepwalking is characterized by a person walking or performing other activities while still asleep, whereas REM Sleep Behavior Disorder is characterized by physical movements, such as kicking or punching.
Can alcohol consumption worsen symptoms of REM Sleep Behavior Disorder?
Yes, alcohol can worsen symptoms and trigger episodes of REM Sleep Behavior Disorder. It is recommended to avoid or limit alcohol consumption if diagnosed with the disorder.
Is REM Sleep Behavior Disorder more common in certain age groups?
It is more common in older adults, with prevalence rates increasing with age. However, it can occur at any age and affect both men and women equally.
Can stress and anxiety be a trigger for REM Sleep Behavior Disorder?
Yes, stress and anxiety can exacerbate symptoms of REM Sleep Behavior Disorder. Practicing stress-management techniques, such as mindfulness or relaxation exercises, may help reduce symptoms.
Does untreated REM Sleep Behavior Disorder always lead to complications?
No, not all cases will lead to complications. However, untreated REM Sleep Behavior Disorder can increase the risk of injury to self or sleeping partners, as well as increase the risk of developing Parkinson’s disease and dementia.